قسطرة الشريان المحيطي Peripheral vascular angioplasty هي إجراء ل علاج مرض الشرايين الطرفية في الساقين Peripheral artery disease.
نظرة عامة على الإجراء
يوسع الإجراء الشرايين الدموية الضيقة التي تعاني من تصلب في الحوض أو الساقين. يمكن أن تساعد قثطرة الشرايين الطرفية على تدفق الدم بشكل أفضل. قد يقلل هذا من آلام الساق أو يساعد على التئام الجروح بشكل أفضل عند مرضى السكري .
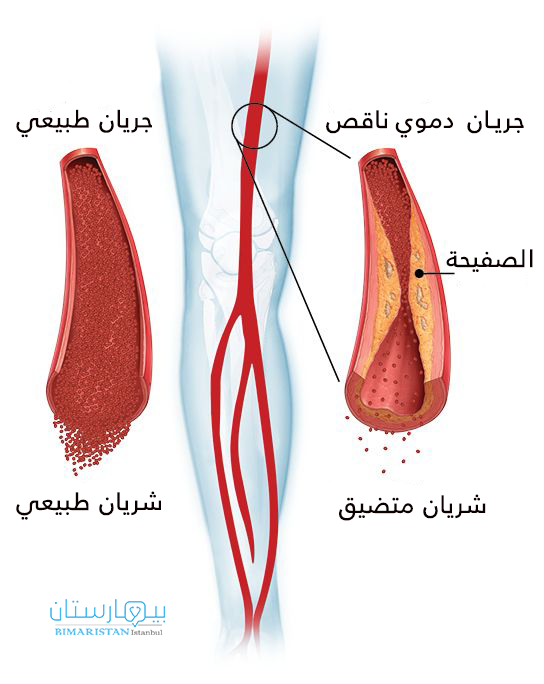
يمكن أن تتضيق الشرايين الطرفية بسبب مادة تسمى اللويحة Plaque، اللويحة هي تراكم للدهون في الشرايين، تحدث في الشرايين الطرفية وأيضا المروية للقلب.
سوف تكون مستيقظا لهذا الإجراء. ستحصل على دواء يمنع الألم ويساعدك على الاسترخاء. أولاً ، سيقوم طبيبك بإجراء اختبار للعثور على الشرايين الطرفية الضيقة. سيضع أنبوبًا صغيرًا في أحد شرايين الفخذ أو الساق. يسمى هذا الأنبوب بالقسطرة. يقوم الطبيب بتحريك القسطرة عبر الشريان ويضع صبغة فيها. تجعل الصبغة الشرايين تظهر في صور الأشعة السينية. يتيح ذلك للطبيب رؤية أي أجزاء ضيقة او انسداد في الشرايين الطرفية .
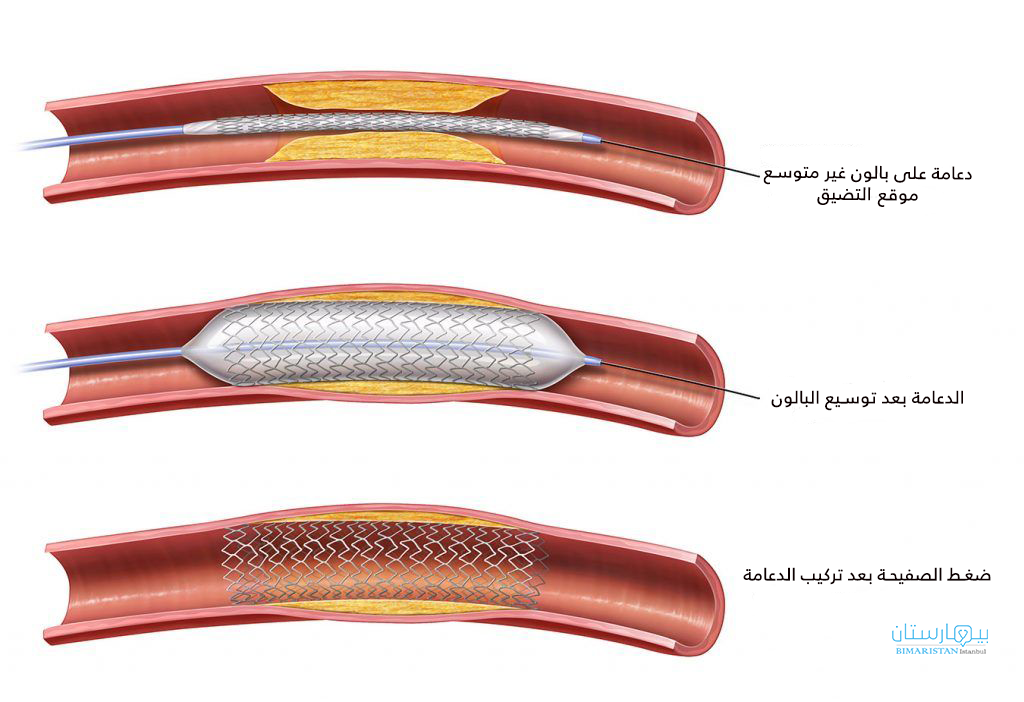
إذا وجد طبيبك تضيق في الشرايين الطرفية او انسداد، فقد يقوم بإجراء قسطرة. للقيام بذلك ، يستخدم الطبيب قسطرة ببالون في طرفه. يذهب إلى الشريان في الفخذ أو الساق. يقوم بتحريك البالون إلى المنطقة الضيقة وينفخها. يضغط البالون على اللويحة على جدران الشريان. هذا يوفر مساحة أكبر لتدفق الدم. قد يقوم الطبيب أيضًا بوضع دعامة بواسطة القسطرة في الشريان، Stent. الدعامة عبارة عن أنبوب صغير يساعد في إبقاء الشريان مفتوحًا. يمكن أن يكون علاج يمنع أيضًا قطع صغيرة من اللويحة من التكسر والتسبب في أمراض في الأوعية الدموية و انسداد شرايين الساق الطرفية .
بعد علاج انسداد الشرايين بالقسطرة قد تحتاج إلى قضاء الليل في المستشفى. لمدة يوم أو يومين بعد العملية ، سوف تحتاج إلى الاسترخاء في المنزل.
تواصل معنا الآن واحجز موعدك مع افضل أطباء قسطرة الشرايين الطرفية والمختصين بأمراض الشرايين الطرفية في تركيا
استطبابات القسطرة العلاجية الطرفية
يشيع استخدام هذا الإجراء لفتح الشرايين الضيقة التي تمد القلب بتدفق الدم (قسطرة القلب) . يمكن استخدامه في أقسام قصيرة من الشرايين االطرفية الضيقة في الأشخاص المصابين بمرض الشرايين الطرفية (PAD) بسبب تصلب الشرايين.
لماذا يتم تنفيذ الإجراء (قسطرة الشرايين الطرفية)؟
تتمثل أعراض انسداد شرايين الساق بسبب تصلب الشرايين في وجود ألم أو وجع أو ثقل في ساقك يبدأ أو يزداد سوءًا عند المشي.
قد لا تحتاج إلى القسطرة الطرفية لأمراض الشرايين الطرفية إذا كان لا يزال بإمكانك القيام بمعظم أنشطتك اليومية. قد يطلب منك مقدم الرعاية الصحية تجربة الأدوية والعلاجات الأخرى أولاً التي قد تساعد في علاج أمراض الأوعية الدموية الطرفية والشرايين الطرفية قبل الحاجة الى قسطرة شرايين.
أسباب إجراء هكذا جراحة في أمراض الشرايين الطرفية هي:
- لديك أعراض تمنعك من القيام بالمهام اليومية. لا تتحسن أعراضك مع العلاجات الطبية الأخرى.
- لديك تقرحات جلدية أو جروح في الساق أو القدم لا تتحسن.
- لديك عدوى أو غرغرينا في ساقك بسبب تصلب الشرايين وقلة تدفق الدم للأطراف.
- لديك ألم في ساقك ناتج عن ضيق و انسداد الشرايين الطرفية، حتى أثناء الراحة.
قبل إجراء عملية الرأب الوعائي ( قسطرة الشرايين الطرفية ) في مرض الشرايين المحيطية، ستخضع لاختبارات خاصة لمعرفة مدى الانسداد في الأوعية الدموية الطرفية
وصف عملية قسطرة الشرايين الطرفية
يستخدم رأب الأوعية الدموية (قسطرة الشرايين الطرفية) Peripheral vascular angioplasty “بالونًا” طبيًا لتوسيع الشرايين الطرفية المسدودة المصابة بتصلب الشرايين. يضغط البالون على الجدار الداخلي للشريان لفتح تصلب الشرايين وتحسين تدفق الدم. غالبًا ما يتم وضع دعامة معدنية Stent عن طريق القسطرة عبر جدار الشريان لمنع تضيق الشرايين الطرفية مرة أخرى.
لعلاج انسداد الشرايين الطرفية في ساقك ، يمكن إجراء قسطرة الشرايين الطرفية في ما يلي:
- الشريان الأورطي (الشريان الرئيسي الذي يأتي من القلب)
- شريان في الورك أو الحوض
- قصور الشرايين في فخذك
- شريان خلف ركبتك
- والشرايين الطرفية في أسفل ساقك

تساعد قثطرة الشرايين الطرفية على تدفق الدم بشكل أفضل، قد يقلل هذا من آلام الساق أو يساعد على التئام الجروح بشكل أفضل.
ما عليك توقعه أثناء إجراء قسطرة الشرايين والأوعية الدموية الطرفية
- سيتم إعطاؤك دواء لمساعدتك على الاسترخاء. ستكون مستيقظا ولكن نعسان.
- قد يتم إعطاؤك أيضًا دواء مضاد لتخثر الدم لمنع تجلط الدم.
- سوف تستلقي على ظهرك على طاولة عمليات مبطنة. سيحقن الجراح بعض الأدوية المخدرة في المنطقة التي سيتم علاجها حتى لا تشعر بالألم. وهذا ما يسمى بالتخدير الموضعي.
سيقوم بعد ذلك إبرة دقيقة في الأوعية الدموية الطرفية في الفخذ. سيتم إدخال سلك مرن صغير من خلال هذه الإبرة باتجاه الشرايين الطرفية المصابة ب تصلب الشرايين
- سيتمكن جراح القسطرةمن رؤية الشريان باستخدام صور الأشعة السينية الحية. سيتم حقن صبغة في جسمك لإظهار تدفق الدم عبر الشرايين الطرفية. ستجعل الصبغة من السهل رؤية منطقة انسداد الشرايين الطرفية ( تصوير الشرايين).
- سيقوم الجراح بإدخال قسطرة عبر الشريان إلى منطقة انسداد الشرايين الطرفية.
- بعد ذلك ، سيقوم الجراح بتمرير سلك توجيه عبر القسطرة التداخليةإلى منطقة انسداد الشرايين الطرفية.
- سيدفع الجراح قسطرة أخرى ببالون صغير جدًا في نهايته فوق السلك التوجيهي وفي المنطقة المسدودة من الشرايين الطرفية..
- يُملأ بالون القسطرة بعد ذلك بسائل التباين لنفخ البالون. هذا يفتح الأوعية الدموية والشرايينالمسدودة ويعيد تدفق الدم إلى القلب.
يمكن أيضًا وضع دعامة في المنطقة المسدودة. يتم إدخال الدعامة في نفس الوقت مع قسطرة البالون. يتمدد عندما ينفجر البالون. تُترك الدعامة في مكانها للمساعدة في إبقاء الشريان مفتوحًا. ثم يتم إزالة البالون وجميع أسلاك القسطرة
قبل الإجراء
خلال أسبوعين قبل الجراحة:
- أخبر مقدم الخدمة عن الأدوية التي تتناولها ، حتى الأدوية ، أو المكملات الغذائية ، أو الأعشاب التي اشتريتها بدون وصفة طبية.
- أخبري مقدم الخدمة إذا كنت تعانين من حساسية تجاه المأكولات البحرية ، أو إذا كان لديك رد فعل سيئ تجاه مادة التباين (الصبغة) أو اليود في الماضي المستخدمة في قسطرة الأوعية الدموية، أو إذا كنت حاملاً أو يمكن أن تكوني حاملاً.
- أخبر مقدم الخدمة الخاص بك إذا كنت تتناول سيلدينافيل (فياجرا) أو فاردينافيل (ليفيترا) أو تادالافيل (سياليس).
- أخبر مقدم الخدمة إذا كنت تشرب الكثير من الكحول (أكثر من مشروب أو مشروبين في اليوم).
- قد تحتاج إلى التوقف عن تناول الأدوية التي تزيد من صعوبة تخثر الدم قبل أسبوعين من الجراحة. وتشمل هذه الأسبرين وإيبوبروفين (أدفيل وموترين) وكلوبيدوجريل (بلافيكس) ونابروسين (أليف ونابروكسين) وأدوية أخرى مثل هذه.
- اسأل عن الأدوية التي يجب أن تتناولها في يوم الجراحة.
- إذا كنت تدخن ، يجب أن تتوقف. اطلب من مزودك المساعدة.
- أخبر مقدم الخدمة دائمًا عن أي نزلة برد أو إنفلونزا أو حمى أو هربس أو أي مرض آخر قد تعاني منه قبل الجراحة.
لا تشرب أي شيء بعد منتصف الليل في الليلة السابقة للجراحة ، بما في ذلك الماء.
في يوم الجراحة
- تناول الأدوية التي طلب منك مزودك تناولها مع رشفة صغيرة من الماء.
- سيتم إخبارك بموعد الوصول إلى المستشفى..
بعد العملية
بعد الإجراء ، سيتم الضغط على المنطقة التي تم وضع القسطرة فيها في الأوعية الدموية. ثم يمكن تغطية المنطقة بضمادة أو جهاز ضغط. هذا سيمنع النزيف. ستقوم الممرضات بفحص معدل ضربات القلب وضغط الدم. ستفحص الممرضة أيضًا موقع القسطرة بحثًا عن النزيف.
سوف تحتاج إلى الاستلقاء والحفاظ على ساقك مستقيمة لعدة ساعات. قد تضع الممرضة كيسًا ثقيلًا على ساقك لإبقائها ثابتة.
يستطيع العديد من الأشخاص العودة إلى منازلهم من المستشفى في غضون يومين أو أقل. بعض الناس قد لا يضطرون حتى إلى البقاء بين عشية وضحاها. يجب أن تكون قادرًا على التجول في غضون 6 إلى 8 ساعات بعد الإجراء. قد يكون لديك كدمة أو كتلة صغيرة حيث تم وضع القسطرة في الأوعية الدموية. هذا أمر طبيعي وسيختفي.
سيشرح لك مزودك كيفية الاعتناء بنفسك.
مدى فعالية الإجراء
يمكن أن يساعد رأب الأوعية الدموية في الشريان المحيطي Peripheral vascular angioplastyعلى استعادة تدفق الدم وتخفيف العرج المتقطع.
تعتمد جودة عمل القسطرة على حجم الأوعية الدموية وطول الأوعية الدموية المصابة وما إذا كان الأوعية الدموية مسدودة تمامًا.
بشكل عام ، تعمل القسطرة بشكل أفضل في:
- الشرايين الكبيرة.
- الشرايين ذات المساحات الضيقة القصيرة.
- الشرايين الضيقة وغير المسدودة.
المخاطر
تشمل المضاعفات المتعلقة بالقسطرة ما يلي:
- ألم وتورم وحنان في موضع إدخال القسطرة.
- تهيج الوريد بواسطة القسطرة (التهاب الوريد الخثاري السطحي).
- نزيف في موضع القسطرة.
- كدمة حيث تم إدخال القسطرة. هذا عادة ما يختفي في غضون أيام قليلة.
نادرًا ما تحدث مضاعفات خطيرة. قد تشمل هذه المضاعفات:
- الإغلاق المفاجئ للشريان.
- جلطات الدم.
- تمزق صغير في البطانة الداخلية للشريان.
- رد فعل تحسسي تجاه مادة التباين المستخدمة في فحص الشرايين.
- تلف الكلى. في حالات نادرة ، يمكن أن تتسبب مادة التباين في تلف الكلى ، مما قد يؤدي إلى فشل كلوي.
مخاطر الإشعاع
هناك دائمًا خطر طفيف لتلف الخلايا أو الأنسجة من التعرض لأي إشعاع ، بما في ذلك المستويات المنخفضة من الأشعة السينية المستخدمة في هذا الاختبار. لكن خطر التلف من الأشعة السينية يكون عادةً منخفضًا جدًا مقارنة بالفوائد المحتملة للاختبار.

