سرطان الثدي يعتبر أكثر أنواع السرطان انتشاراً لدى النساء وثاني أكثر مسبب للوفاة بعد سرطان الرئة، تعرف على تفاصيل أكثر حول طرق التشخيص والعلاج في تركيا.
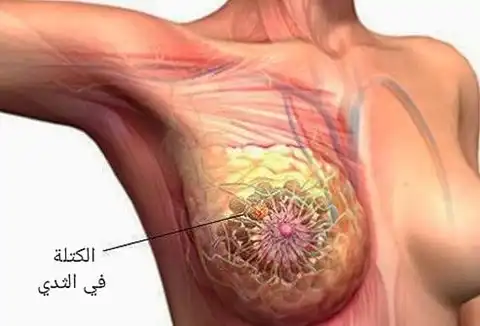
يحدث سرطان الثدي عندما تنمو الخلايا في ثديك وتنقسم بطريقة خارجة عن السيطرة، مما يؤدي إلى تكوين كتلة من الأنسجة تسمى الورم، يزيد خطر الإصابة به مع تقدمك في العمر ومع زيادة الوزن كذلك.
يمكن أن تشمل علامات ورم الثدي الشعور بوجود كتلة في الثدي، مع تغير حجمه، ورؤية تغيرات في جلد الثديين.
إن الكشف المبكر يتم عن طريق إجراء فحص الماموغرام.
ما هو سرطان الثدي breast cancer؟
تنقسم الخلايا cells في الجسم عادة وتتكاثر فقط عند الحاجة إلى خلايا جديدة.
في بعض الأحيان، يحدث انقسام ونمو للخلايا خارج نطاق السيطرة، مما يؤدي إلى تكوين كتلة من الأنسجة تسمى الورم.
إذا كانت الخلايا التي تنمو خارج نطاق السيطرة خلايا طبيعية، فإن الورم يسمى حميد (غير سرطاني).
وأما إذا كانت الخلايا التي تنمو خارج نطاق السيطرة غير طبيعية ولا تعمل مثل خلايا الجسم الطبيعية، فإن الورم يسمى خبيث (سرطاني).
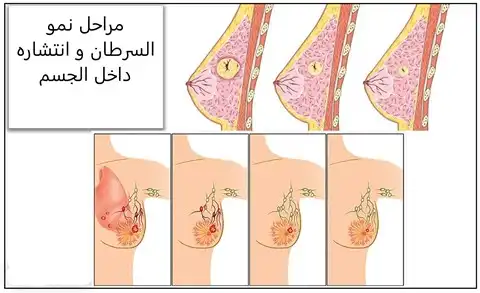
وبشكل مشابه مع الأنواع الأخرى للسرطان، يمكن أن يغزو سرطان الثدي وينمو في الأنسجة المحيطة به.
كما يمكن أن ينتقل أيضًا إلى أجزاء أخرى من الجسم ويشكل أورامًا جديدة، وهي عملية تسمى هجرة الخلايا السرطانية.
من يصاب ﺑﺳرطﺎن اﻟﺛدي ؟
سرطان الثدي هو أكثر أنواع السرطانات شيوعا بين نساء العالم.
حيث يعد التقدم في العمر عامل الخطر الأكثر شيوعًا للإصابة بسرطان الثدي، حيث يتم تشخيص 66٪ من مرضى سرطان الثدي بعد سن 55.
في الولايات المتحدة، يحتل سرطان الثدي المركز الثاني كمسبب لوفاة السيدات بعد سرطان الرئة، وهو السبب الرئيسي للوفاة بالسرطان بين النساء اللائي تتراوح أعمارهن بين 35 و54 عامًا.
تحدث 5 إلى 10٪ فقط من سرطانات الثدي لدى النساء اللاتي لديهن استعداد وراثي واضح للإصابة بالمرض.
غالبية حالات سرطان الثدي عشوائية متفرقة، مما يعني عدم وجود طفرة جينية حاسمة.
هل يصيب سرطان الثدي النساء من جميع الأعراق بالتساوي؟
جميع النساء خاصة مع تقدمهن في السن معرضات لخطر الإصابة بسرطان الثدي.
لا تنتشر مخاطر الإصابة بسرطان الثدي بشكل عام بالتساوي بين المجموعات العرقية، وتختلف المخاطر بين المجموعات العرقية لأنواع مختلفة من سرطان الثدي.
انخفضت معدلات وفيات سرطان الثدي في الولايات المتحدة بنسبة 40٪ منذ عام 1989، لكن الفوارق مستمرة وتتسع بين النساء السود غير اللاتينيين والنساء البيض من غير اللاتينيين.
هل ظهور أورام الثدي الحميدة يعني أن احتمالية الإصابة بسرطان الثدي أعلى؟
نادرًا ما تزيد أورام الثدي الحميدة من خطر الإصابة ب سرطان الثدي (الأورام الخبيثة).
بعض النساء لديهن تظهر لديهم كتل تكون نتيجة الخزعة لديهم هي (نمو الخلايا المفرط). حيث تزيد هذه الحالة من مخاطر حدوث السرطان بشكل طفيف.
عندما تُظهر الخزعة تضخمًا وخلايا غير طبيعية، وهي حالة تسمى تضخم غير نمطي، فإن خطر الإصابة بسرطان الثدي يزيد إلى حد ما.
ما هي أنواع سرطان الثدي؟
أكثر أنواع سرطان الثدي شيوعاً هي:
سرطان الأقنية الغازي:
يبدأ هذا السرطان في قنوات الحليب بالثدي ثم يخترق جدار القناة ويغزو الأنسجة المحيطة بالثدي.
هذا هو الشكل الأكثر شيوعًا لسرطان الثدي، ويمثل 80٪ من الحالات.
سرطان الأقنية الموضعي:
هو سرطان الأقنية في مرحلته الأولى، يشير مصطلح “الموضعي” إلى حقيقة أن السرطان لم ينتشر إلى ما بعد نقطة نشأته.
فهو في هذه الحالة، يقتصر المرض على قنوات الحليب ولم يغز أنسجة الثدي القريبة.
إذا لم يتم علاجه، فقد يصبح سرطان الأقنية الموضعي سرطانًا جائرًا.
أهمية الكشف المبكر أنه قابل للشفاء دائمًا تقريبًا.
السرطان الفصيصي الغازي:
يبدأ هذا السرطان في فصيصات الثدي حيث يتم إنتاج حليب الثدي، ولكنه ينتشر إلى الأنسجة المحيطة بالثدي.
يمثل 10 إلى 15٪ من سرطانات الثدي، يمكن أن يكون تشخيص هذا السرطان أكثر صعوبة من خلال تصوير الثدي بالأشعة السينية.
السرطان الفصيصي الموضعي:
هو علامة على السرطان الموجود فقط في فصيصات الثدي.
إنه ليس سرطانًا حقيقيًا، ولكنه بمثابة علامة على زيادة احتمال الإصابة بسرطان الثدي لاحقًا، ربما في كلا الثديين أو في أحدهما.
وبالتالي من المهم للنساء المصابات بالسرطان الفصيصي إجراء فحوصات سريرية للثدي وتصوير الإشعاعي للثدي بالأشعة السينية.
ما هو سرطان الثدي الغازية؟
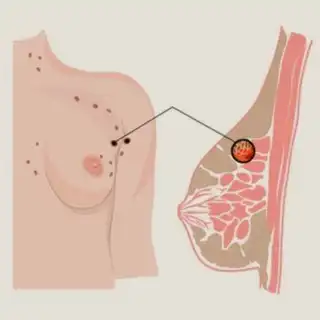
يحدث سرطان الثدي الغازي عندما تنتشر الخلايا خارج القنوات أو الفصيصات، تغزو هذه الخلايا أولاً أنسجة الثدي المحيطة، ويمكن أن تنتقل إلى العقد اللمفاوية.
هل يمكن أن يتشكل السرطان في أجزاء أخرى من الثدي؟
يمكن أن تتكون السرطانات أيضًا في أجزاء أخرى من الثدي، ولكن هذه الأنواع من السرطان أقل شيوعًا عادةً ويمكن أن تشمل:
الساركوما الوعائية:
يبدأ هذا النوع من السرطان في الخلايا التي تتكون منها بطانة الأوعية الدموية أو الأوعية اللمفاوية.
يمكن أن تبدأ هذه السرطانات في أنسجة الثدي أو جلد الثدي وهذا نادر.
وسرطان الثدي الالتهابي:
هذا النوع من السرطان نادر أيضاً ويختلف عن الأنواع الأخرى من سرطان الثدي وهو ناتج عن الخلايا السرطانية التي تسد الأوعية اللمفاوية للجلد مما يسبب تورم بال ثدي واحمراره.
مرض باجيت للثدي:
المعروف أيضًا بمرض باجيت الذي يصيب حلمة الثدي، يؤثر هذا السرطان على جلد الحلمة والهالة (الجلد حول الحلمة).
أورام فيلوديس:
هذه نادرة ومعظمها كتل ليست سرطانية (أورام حميدة) وبعضها سرطاني، تبدأ هذه الأورام في النسيج الضام للثدي، وهو ما يسمى السدى.
ما هي مراحل سرطان الثدي؟
يوجد نوعان من أنظمة التصنيف لسرطان الثدي أحدهما هو “التصنيف التشريحي” والآخر هو “التصنيف التنبؤي”.
يتم تحديد المرحلة التشريحية من خلال معرفة مناطق الجسم التي يوجد فيها سرطان الثدي كما يساعد في تحديد العلاج الأنسب.
يساعد التصنيف التنبؤوي الفريق الطبي المتخصص على توقع احتمالية شفاء المريضة من سرطان الثدي بعد تقديم العلاج المناسب.
ولفهم مراحل سرطان الثدي بشكل أكثر أقرأ المقال التالي
أعراض وأسباب سرطان الثدي
ما هي أسباب سرطان الثدي؟
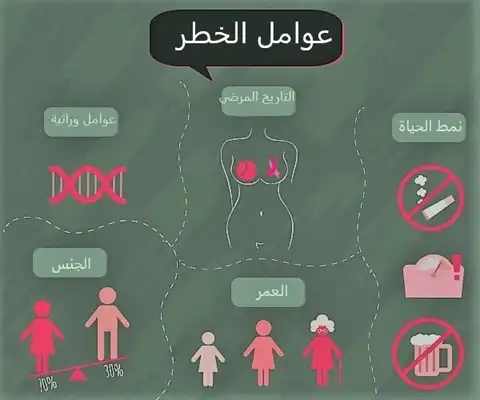
عملياً إلى الآن لا يُعرف ما الذي يسبب هذا النوع من السرطان، ولكن يوجد العديد عوامل الخطر التي تزيد احتمال الاصابة بسرطان الثدي حيثُ أن عمر المرأة وبعض العوامل الوراثية والتاريخ الطبي العائلي والتاريخ الصحي الشخصي والنظام الغذائي ﻓﻲ خطر الإصابة بسرطان الثدي.
ما هي عوامل خطر الإصابة بسرطان الثدي؟
حيث أن هذه العوامل تزيد من احتمالية حدوث السرطان على الرغم من أن وجدها جميعاً لا يعني حتمية اصابتك بالسرطان.
عوامل الخطر التي يمكن السيطرة عليها لسرطان الثدي
استهلاك الكحول: والذي يزيد من احتمال الإصابة بسرطان الثدي بزيادة كمية الكحول المستهلكة.
الزيادة بوزن الجسم: تعد السمنة عامل من عوامل الخطر للإصابة بسرطان الثدي. حيث أنه من المهم تناول نظام صحي والالتزام بممارسة الرياضة.
زراعة الثدي (تكبير الثدي): إن عملية تكبير الثدي باستخدام االسيليكون و تشكل الندبات الناتجة عن العملية تجعل من الصعب تمييز الأنسجة السرطانية المتشكلة.
كما يمكن أن يتشكل سرطان نادر يسمى سرطان الغدد الليمفاوية ذو الخلايا الكبيرة (ALCL) المرتبط بالزرعات.
عدم الرضاعة: إن عدم الرضاعة قد تؤدي إلى زيادة خطر الإصابة بسرطان الثدي.
استخدام الأدوية الهرمونية: يتضمن هذا استخدام العلاج بالهرمونات التي تستخدم بعد انقطاع الطمث والأدوية المانعة للحمل.
عوامل الخطر التي لا يمكن السيطرة عليها لسرطان الثدي
الجنس: يعتبر سرطان الثدي أكثر شيوعاً عند النساء بالرغم من امكانية اصابة الرجال.
أنسجة ثدي عالية الكثافة: يعتبر الثدي عالي الكثافة أكثر عرضة للاصابة بالسرطان كما أنه يجعل من الصعب رؤية الأورام أثناء تصوير الثدي بالأشعة السينية.
عوامل الإنجاب: تشمل بدء الدورة الشهرية في مرحلة مبكرة من العمر (قبل سن الـ12) أو الدخول في سن الياس بعد سن ال55، أو عدم انجاب الأطفال، أو إنجاب الطفل الأول بعد سن الـ30 عامًا.
التقدم في السن: معظم الأشخاص المصابين قد تجاوز عمرهم ال55 سنة.
التعرض للإشعاع: حيث يمكن أن ينتج هذا النوع من السرطان عند التعرض للأشعة السينية أثناء إجراء التنظير أو عند اجراء صور الصدر العادية.
وجود تاريخ عائلي للإصابة بسرطان الثدي، أو وجود طفرات جينية مرتبطة بأنواع معينة من سرطان الثدي:
حيث أن وجود قريب مصاب بسرطان الثدي من الدرجة الأولى (الأم، الأخت، الابنة، الأب، الأخ، الابن) يشكل خطرًا أكثر للإصابة بسرطان الثدي.
كما أنه من حيث الطفرات الوراثية، تشمل هذه الطفرات في المادة الوراثية وجود جينات مثل BRCA1 وBRCA2.
سوابق الإصابة بسرطان الثدي: حيث يكون نسبة الخطر أكبر إذا كنت مصابة مسبقاً ب سرطان الثدي و/ أو أنواع آخرى من أورام الثدي الحميدة مثل سرطان الفصيص المنطقي، أو التضخم الغير نمطي. أو سرطان الأقنية الموضعي.
التعرض لـ ثنائي إيثيل ستيلبوستيرول (DES): تم وصف DES لبعض النساء الحوامل في الولايات المتحدة خلال 1940-1971. وتم ربط تناول هذه المادة مع الإصابة بالسرطان.
ما هي العلامات التحذيرية لسرطان الثدي؟
-اكتشاف كتلة أو سماكة في الثدي أو بالقرب منه أو تحت الإبط تستمر خلال الدورة الشهرية.
-كتلة، قد تبدو صغيرة مثل حبة البازلاء.
-تغيير في شكل أو/ وحجم أو محيط الثدي.
-إفرازات سائلة ملطخة بالدم أو صافية ﻣن الحلمة.
-تغير في شكل أو ملمس جلد الثدي أو الحلمة (مدمّل، أو مجعد، أو متقشر، أو ملتهب).
-احمرار في الجلد على الثدي أو الحلمة.
-منطقة تختلف بشكل واضح عن أي منطقة أخرى في الثديين.
-منطقة صلبة تحت الجلد.
يمكن العثور على هذه التغييرات عند إجراء الفحوصات الذاتية الشهرية للثدي. من خلال إجراء الفحص الذاتي للثدي، يمكنك التعرف على التغيرات الشهرية الطبيعية في ثدييك.
يجب إجراء الفحص الذاتي للثدي في نفس الوقت من كل شهر، بعد ثلاثة إلى خمسة أيام من انتهاء الدورة الشهرية.
إذا كنت في سن الياس، قومي بإجراء الفحص في نفس اليوم من كل شهر.
التشخيص والاختبارات
كيف يتم تشخيص سرطان الثدي؟
أثناء الفحص البدني المنتظم، سيقوم الدكتور بطلب واحد أو أكثر مما يلي:
فحص الثدي:
أثناء فحص الثدي سيتحسس الطبيب بعناية الورم والأنسجة المحيطة به.
عادة ما يكون الشعور بسرطان الثدي مختلفًا (في الحجم والملمس والحركة) عن الكتل الحميدة.
التصوير الشعاعي للثدي :
يمكن أن يوفر اختبار الأشعة السينية للثدي معلومات مهمة حول كتلة الثدي.
التصوير بالموجات فوق الصوتية:
يستخدم هذا الاختبار الموجات الصوتية للكشف عن طبيعة كتلة الثدي – سواء كانت كيسًا مملوءًا بسائل (غير سرطاني) أو كتلة صلبة (قد تكون سرطانية أو لا تكون).
يمكن إجراء ذلك جنبًا إلى جنب مع التصوير الشعاعي للثدي.
بناءً على نتائج هذه الاختبارات، قد يطلب طبيبك خزعة للحصول على عينة من خلايا أو أنسجة كتلة الثدي.
يتم إجراء الخزعات باستخدام الجراحة أو الإبر.
بعد أخذ العينة، يتم إرسالها إلى المختبر حيث يقوم أخصائي علم الأمراض – وهو طبيب متخصص في تشخيص التغيرات غير الطبيعية في الأنسجة – بمشاهدة العينة تحت المجهر والبحث عن أشكال الخلايا أو أنماط النمو غير الطبيعية.
عندما يكون هنالك خلايا سرطان موجودة، يمكن لطبيب علم الأمراض غالباً معرفة نوع السرطان (سرطان الأقنية أو الفصيص) وما إذا كان قد انتشر خارج القنوات أو الفصيصات (الغازية).
يمكن أن تُظهر الاختبارات، مثل اختبارات مستقبلات الهرمونات (الإستروجين والبروجسترون) ومستقبل عامل نمو البشرة البشري (HER2 / neu)، ما إذا كانت الهرمونات أو عوامل النمو تساعد في نمو السرطان.
إذا أظهرت نتائج الاختبار أنها (الاختبار الإيجابي)، فمن المرجح أن يستجيب السرطان للعلاج الهرموني أو العلاج بالأجسام المضادة.
حيث تمنع هذه العلاجات السرطان من الحصول على هرمون الاستروجين وبالتالي تؤدي إلى تضاؤل حجم السرطان.
الاختبارات التشخيصية الأخرى في تركيا
مجموعة من طرق التسخيص الأخرى:
التصويرالومضاني للثدي:
تقنية يتم فيها حقن مادة ظليلة في الوريد بالذراع. يتم التقاط صورة للثدي بكاميرا خاصة تكشف الأشعة (أشعة جاما) المنبعثة من هذه المادة تجمع الخلايا السرطانية، التي تحتوي على أوعية دموية أكثر من الأنسجة الحميدة، حيث تصدر قدرًا أكبر من الصبغة وتظهر الصورة الإجمالية أكثر إشراقًا.
المسح بالتصوير المقطعي بالإصدار البوزيتروني (PET):
تقنية تقيس الإشارة من المواد المشعة المحقونة التي تهاجر إلى الخلايا السرطانية سريعة الانقسام.
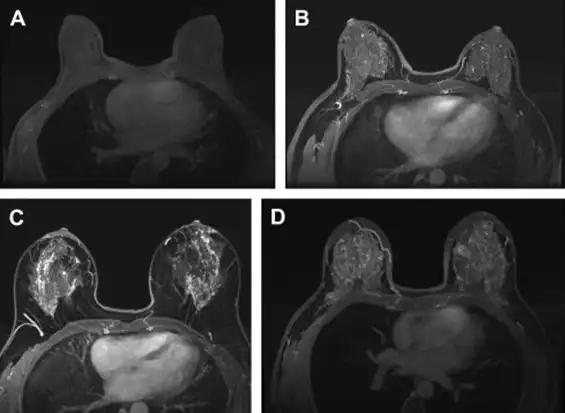
التصوير بالرنين المغناطيسي (MRI):
جهاز ينتج صورًا شديدة الوضوح لجسم الإنسان دون استخدام الأشعة السينية لذا تعد آمنة للحوامل.
علاج سرطان الثدي في تركيا
إذا تم تشخيص سرطان الثدي، فسيقوم الفريق الطبي بوضع خطة علاجية للقضاء عليه، لتقليل فرصة النكس، وكذلك لتقليل فرصة انتقال السرطان إلى مكان خارج الثدي.
يعتمد نوع العلاج الموصى به على حجم وموقع الورم في الثدي، ونتائج الفحوصات المخبرية التي يتم إجراؤها على الخلايا السرطانية، ومرحلة المرض أو مدى انتشاره.
علاجات سرطان الثدي موضعية أو جهازية.
تُستخدم العلاجات الموضعية (كالجراحة والعلاج الشعاعي) لإزالة الخلايا السرطانية أو تدميرها أو السيطرة عليها.
تستخدم العلاجات الجهازية ( العلاج الكيميائي والهرموني) لتدمير الخلايا السرطانية في جميع أنحاء الجسم أو السيطرة عليها.
جراحة استئصال الثدي:
تتضمن جراحة الحفاظ على الثدي إزالة الجزء السرطاني من الثدي ومنطقة الأنسجة الطبيعية المحيطة به، مع السعي للحفاظ على المظهر الطبيعي للثدي تقريباً . غالبًا ما يُطلق على هذا الإجراء اسم استئصال الكتلة الورمية، ويشار إليه أيضًا باسم استئصال الثدي الجزئي.
عادة، يتبع بالعلاج الإشعاعي لعلاج أنسجة الثدي المتبقية.
معظم النساء المصابات بورم صغير في مراحله المبكرة هن مرشحات ممتازات لهذه الطريقة.
يعتبر استئصال الثدي (إزالة الثدي بالكامل) أحد الخيارات أيضاً.
لكن اجراءات استئصال الثدي التي يتم إجراؤها اليوم ليست مثل عمليات استئصال الثدي الجذرية القديمة.
حيث كانت عمليات استئصال الثدي الجذري إجراءات واسعة النطاق تضمنت إزالة أنسجة الثدي والجلد وعضلات جدار الصدر.
أما اليوم وفي تركيا، لا تؤدي إجراءات استئصال الثدي عادةً إلى إزالة العضلات، وبالنسبة للعديد من النساء، يكون استئصال الثدي مصحوبًا إما بإعادة بناء (ترميم) الثدي الفورية أو المتأخرة.
ماذا يحدث بعد علاج سرطانة الثدي الموضعية؟
بعد العلاج الموضعي لسرطان الثدي، سيحدد فريق العلاج احتمالية عودة السرطان خارج الثدي
. قد ينصح طبيب الأورام، باستخدام الأدوية مثل عقار تاموكسيفين أو أناستروزول (ARIMIDEX®) أو ربما العلاج الكيميائي.
تُستخدم هذه العلاجات بالإضافة إلى العلاج الموضعي لسرطان الثدي الجراحي أو الإشعاعي، ولكن ليس بديلاً عنه.
بعد علاج سرطان الثدي، من المهم بشكل خاص أن تستمر المرأة في إجراء فحص الثدي الشهري.
ستساعدك الفحوصات المنتظمة على اكتشاف النكس مبكراً.
فحص الثدي بعد علاج سرطان الثدي
- بعد الجراحة
قد يكون خط الشق (الندبة) سميكًا ومرتفعًا وأحمر اللون وربما يكون مؤلمًا لعدة أشهر بعد الجراحة. تذكر أن تفحص خط الشق بالكامل.
إذا كان هناك احمرار في مناطق بعيدة عن الندبة، فاتصل بطبيبك.
- بعد إعادة بناء الثدي
بعد إعادة بناء الثدي، يتم إجراء فحص الثدي للثدي الذي أعيد بناؤه بنفس الطريقة تمامًا كما هو الحال بالنسبة للثدي الطبيعي.
إذا تم استخدام غرسة لإعادة البناء، فاضغطي بقوة للداخل عند حواف الغرسة لتشعري بالأضلاع تحتها.
إذا تم استخدام أنسجتك الخاصة لإعادة البناء، فقد تشعرين بشكل طبيعي ببعض التنميل في الثديين.
- بعد العلاج الإشعاعي
بعد العلاج الإشعاعي، قد تلاحظين بعض التغييرات في أنسجة الثدي. قد يبدو الثدي أحمر اللون أو مصابًا بحروق وقد يتهيج أو يلتهب.
بمجرد التوقف عن العلاج، سيختفي الاحمرار ويقل التهاب أو تهيج الثدي.
في بعض الأحيان، يمكن أن يصبح الجلد أكثر التهابًا لبضعة أيام بعد العلاج ثم يتحسن تدريجيًا بعد بضعة أسابيع.
أثناء العلاج الإشعاعي، يجب أن تستمر الفحوصات الذاتية الشهرية للثدي المشعع وكذلك الثدي الآخر.
إذا لاحظت أي تطورات جديدة، فاتصلي بطبيبك.
معظم أورام الثدي (حوالي 80 بالمائة) حميدة. ومع ذلك، قد يقودك الفحص الذاتي إلى الكشف المبكر عن سرطان جديد أو ناكس. كلما كان التشخيص مبكرًا، كانت فرص نجاح العلاج أفضل.
الوقاية
كيف يمكنني حماية نفسي من الإصابة بسرطان الثدي؟
اتبع هذه الخطوات الثلاث للاكتشاف المبكر:
احصل على صورة ماموجرام: حيث توصي جمعية السرطان الأمريكية بإجراء تصوير الثدي بالأشعة كل عام بعد سن 40.
افحصي ثدييك كل شهر بعد سن العشرين. سوف تتعرفين على ملامح ثدييك وستكونين أكثر انتباهاً للتغييرات.
قومي بفحص ثديك عند الطبيب مرة واحدة على الأقل كل ثلاث سنوات بعد سن 20، وكل عام بعد سن 40.
يمكن أن تكشف فحوصات الثدي السريرية عن الكتل التي قد لا يتم اكتشافها بواسطة تصوير الثدي الشعاعي.
هل يمكن أن تساعد التمارين الرياضية في تقليل خطر اصابتي بسرطانات الثدي؟
ممارسة الرياضة جزء كبير من أسلوب الحياة الصحي.
يمكن أن يكون أيضًا وسيلة مفيدة لتقليل خطر الإصابة بسرطان الثدي في سنوات ما بعد انقطاع الطمث.
غالبًا ما تكتسب النساء الوزن أثناء انقطاع الطمث.
الأشخاص الذين لديهم كميات كبيرة من الدهون في الجسم أكثر عرضة للإصابة بسرطان الثدي.
ومع ذلك، من خلال تقليل الدهون في الجسم من خلال ممارسة الرياضة، قد تتمكن من تقليل خطر الإصابة بسرطان الثدي.
التوصية العامة لممارسة الرياضة بانتظام هي حوالي 150 دقيقة كل أسبوع. هذا يعني أنك تتمرن لمدة 30 دقيقة، خمسة أيام كل أسبوع.
ومع ذلك، فإن مضاعفة مقدار التمرين الأسبوعي إلى 300 دقيقة (60 دقيقة، خمسة أيام كل أسبوع) يمكن أن يفيد النساء بعد انقطاع الطمث بشكل كبير.
تسمح لك مدة التمرين الأطول بحرق المزيد من الدهون، وتحسين، وظائف القلب، والرئتين.
يمكن أن يختلف نوع التمرين الذي تقوم به – الهدف الرئيسي هو رفع معدل ضربات قلبك أثناء ممارسة الرياضة.
من المستحسن أن يرتفع معدل ضربات قلبك بحوالي 65 إلى 75٪ من الحد الأقصى لمعدل ضربات القلب أثناء التمرين.
يمكنك معرفة الحد الأقصى لمعدل ضربات القلب بطرح عمرك الحالي من 220. إذا كان عمرك 65، على سبيل المثال، فإن الحد الأقصى لمعدل ضربات قلبك هو 155.
تعتبر التمارين الهوائية طريقة رائعة لتحسين وظائف القلب والرئتين، وكذلك حرق الدهون. تتضمن بعض التمارين الهوائية التي يمكنك تجربتها ما يلي:
المشي/ السباحة/ الجري/ ركوب الدراجة/ الرقص.
اختاري نشاطًا تستمتعين به وتريدين القيام به مرارًا وتكرارًا.
كلما أحببت نشاطك، زادت احتمالية مواصلتك لممارسة الرياضة يومًا بعد يوم.
لا يتعين عليك القيام بنفس النشاط طوال 300 دقيقة من تمرينك الأسبوعي. يمكنك مزجها وتجربة أشياء مختلفة على مدار الأسبوع.
الشيء المهم هو الاستمرار في التحرك.
تذكر أن هناك العديد من الفوائد لممارسة المزيد من التمارين في روتينك الأسبوعي. يمكن أن تشمل بعض فوائد التمارين الهوائية:
- خفض الكوليسترول وضغط الدم.
- زيادة القدرة على التحمل.
- فقدان الوزن أو الحفاظ على وزنك الحالي.
- تخفيف التوتر.
- النوم الجيد.
إليك مقال يوضح كيفية المتابعة بعد سرطان الثدي
كيف يقلل عقار تاموكسيفين، ورالوكسيفين، وأناستروزول، وإكسيميستان من خطر الإصابة بسرطان الثدي؟
إذا كنت في خطر متزايد للإصابة بسرطان الثدي، فقد تساعد أربعة أدوية – تاموكسيفين (Nolvadex®)، ورالوكسيفين (Evista®)، وأناستروزول (Arimidex®)، وإكسيميستان (Aromasin®) – في تقليل خطر الإصابة بهذا المرض.
تعمل هذه الأدوية فقط لتقليل خطر الإصابة بنوع معين من سرطان الثدي يسمى سرطان الثدي الإيجابي لمستقبلات هرمون الاستروجين.
يمثل هذا النوع من سرطان الثدي حوالي ثلثي جميع أنواع سرطان الثدي.
يعتبر التاموكسيفين ورالوكسيفين من الأدوية التي تسمى مُعدِّلات مستقبلات هرمون الاستروجين الانتقائية (SERMs).
حيث تعمل هذه الأدوية عن طريق منع تأثيرات هرمون الاستروجين في أنسجة الثدي عن طريق الارتباط بمستقبلات هرمون الاستروجين في خلايا الثدي.
نظرًا لأن SERMs ترتبط بالمستقبلات، يتم حظر هرمون الاستروجين من الارتباط. هرمون الاستروجين هو الوقود الذي يجعل معظم خلايا سرطان الثدي تنمو.
استخدام هذه الأدوية يمنع تطور سرطان الثدي الإيجابي لمستقبلات هرمون الاستروجين.
يقع Anastrozole و exemestane في فئة من الأدوية تسمى مثبطات الأروماتاز (AIs).
حيث تعمل هذه الأدوية عن طريق منع إنتاج هرمون الاستروجين. تقوم مثبطات الأروماتاز بذلك عن طريق منع نشاط إنزيم يسمى أروماتاز ، وهو ضروري لصنع الإستروجين.
إلى أي مدى يقلل عقار تاموكسيفين ورالوكسيفين من خطر الإصابة ؟
أظهرت دراسات متعددة أن كل من عقار تاموكسيفين ورالوكسيفين يمكن أن يقلل من خطر الإصابة بسرطان الثدي الإيجابي لمستقبلات هرمون الاستروجين لدى النساء الأصحاء بعد سن اليأس و المعرضات لخطر الإصابة بالمرض.
خفض تاموكسيفين الخطر بنسبة 50 في المئة.
خفض رالوكسيفين المخاطر بنسبة 38 في المئة.
بشكل عام، أظهرت النتائج المجمعة لهذه الدراسات أن تناول عقار تاموكسيفين أو رالوكسيفين يوميًا لمدة خمس سنوات يقلل من خطر الإصابة بسرطان الثدي بنسبة الثلث على الأقل.
في إحدى التجارب التي قارنت عقار تاموكسيفين مباشرة مع رالوكسيفين، وجد أن الرالوكسيفين أقل فعالية قليلاً من عقار تاموكسيفين للوقاية من سرطان الثدي.
تمت الموافقة على استخدام كل من عقار تاموكسيفين ورالوكسيفين لتقليل خطر الإصابة بسرطان الثدي لدى النساء المعرضات لخطر الإصابة بالمرض.
تمت الموافقة على عقار تاموكسيفين للاستخدام في كل من النساء في فترة ما قبل انقطاع الطمث والنساء بعد انقطاع الطمث.
تمت الموافقة على استخدام رالوكسيفين فقط في النساء بعد سن الياس.
إلى أي مدى يقلل عقار أناستروزول وإكسيميستان من خطر الإصابة بورم الثدي؟
أظهرت الدراسات أن كلا من أناستروزول وإكسيميستان يمكن أن يقلل من خطر الإصابة بورم الثدي لدى النساء بعد سن اليأس المعرضات لخطر متزايد للإصابة بالمرض.
في إحدى الدراسات الكبيرة، أدى تناول عقار اناستروزول لمدة خمس سنوات إلى خفض خطر الإصابة بسرطان الثدي الإيجابي لمستقبلات هرمون الاستروجين بنسبة 53 بالمائة.
في دراسة أخرى، أدى تناول إكسيميستان لمدة ثلاث سنوات إلى خفض خطر الإصابة بسرطان الثدي الإيجابي لمستقبلات هرمون الاستروجين بنسبة 65 في المائة.
الآثار الجانبية الأكثر شيوعًا مع أناسترازول وإكسيميستان هي آلام المفاصل، وانخفاض كثافة العظام، وأعراض انقطاع الطمث (مثل الهبات الساخنة، والتعرق الليلي، وجفاف المهبل).
يبقى مركز بيمارستان الطبي خيارك الأول للعلاج في تركيا.
نوجهك لأفضل الاختصاصين الخبراء بكافة المجالات، نكسر حاجز اللغة أطباء متخصصين عرب سيساعدونك في التواصل مع طبيبك، نساعدك بحجز الموعد بأهم وأحدث المشافي في تركيا.
نقدم خدماتنا على امتداد تركيا وبشكل خاص في اسطنبول ، فالمكان الأفضل بتقديم العلاج لك هو وجهتنا.
نرافقك خطوة بخطوة نحو الشفاء.
استشارات مجانية على مدار الساعة.
لا تتردد بالتواصل معنا، مركز بيمارستان عائلتك في تركيا. يمكنك أن تقرأ عن أنواع أخرى من السرطانات التناسلية لدى النساء وطرق علاجها في تركيا.

