تعتبر عملية زراعة الكبد في تركيا العلاج الجراحي المحدد لمرضى المرحلة النهائية من أمراض الكبد ومرضى الفشل الكبدي الحاد والذي يحسن وظائف الكبد والبقاء على قيد الحياة بعد الزرع.
إن عملية زراعة الكبد هي حل نهائي للعديد من المشاكل الكبدية، حيث أن هذه العملية تنقذ حياة المرضى المصابين بالفشل الكبدي الحاد، وأضرار زراعة الكبد يمكن تلافيها مع تقدم الطب في تركيا.
فما هي نسبة نجاح عملية زراعة الكبد؟ وكم ساعة تستغرق عملية التبرع بالكبد؟ وما هي موانع وشروط عملية زراعة الكبد؟ وهل التبرع بالكبد خطير؟ تعرف معنا على إجابة هذه الأسئلة في المقال التالي.
مقدمة عن عملية زراعة الكبد
تم إجراء أول عملية زرع الكبد عام 1963 في الولايات المتحدة من قبل الجراح توماس سترازل (Thomas Starzl)، وهذه العملية اليوم هي العلاج الأكثر فعالية لحالات فشل الكبد في المرحلة النهائية وحالات الفشل الكبدي الحاد، وقد تم إجراء زرع الكبد لأكثر من 80000 مريض يعانون من الفشل الكبدي المزمن في العالم.
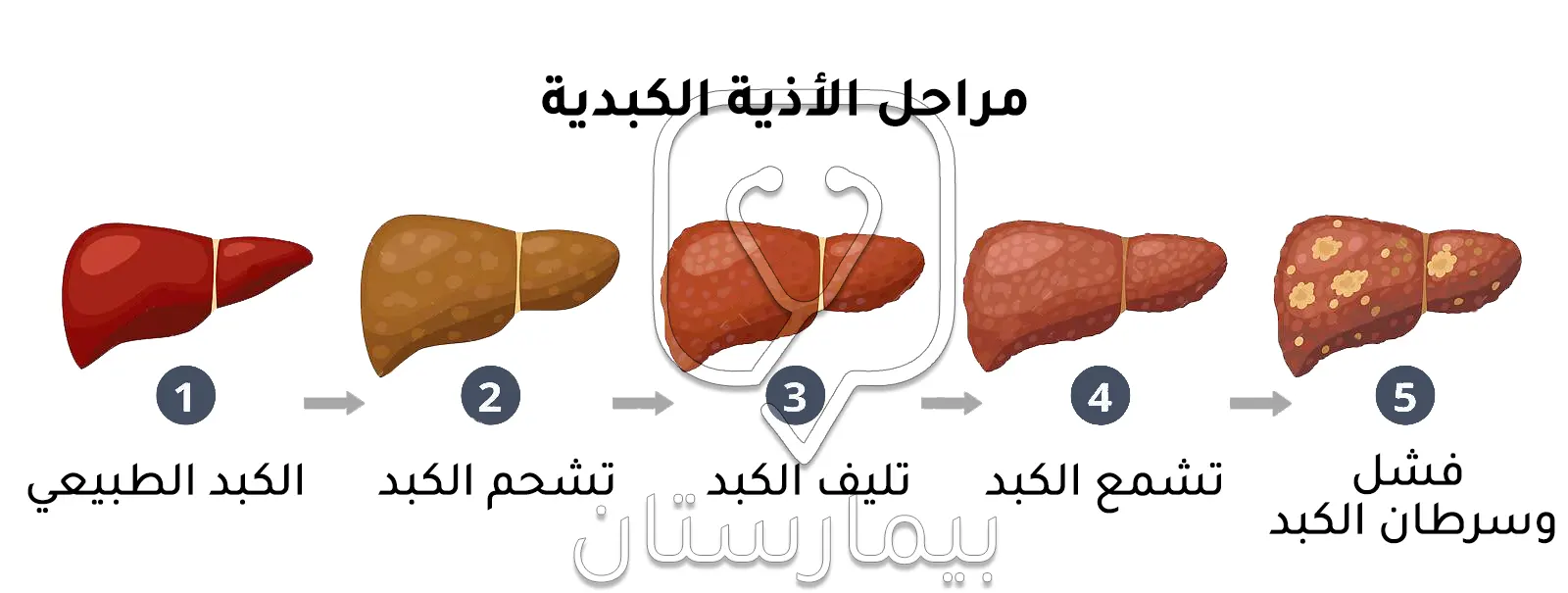
لقد بات زراعة الكبد على مدى العقود الثلاثة الماضية خياراً لإنقاذ حياة المرضى الذين يعانون من أمراض الكبد في مراحل أخيرة، أورام الكبد الخبيثة، الأمراض الاستقلابية المترافقة بأذية الكبد، والفشل الكبدي الحاد، وتهدف عمليات الزرع إلى إطالة عمر المتلقي وتحسين نوعية حياته.
ارتفعت معدلات البقاء على قيد الحياة بعد عملية زراعة الكبد بشكل كبير في الآونة الأخيرة فقد بلغت نسبة البقيا لعام واحد 96% ولعشر سنوات 71% بعد الزرع، فبالإضافة إلى التطورات العديدة في التقنيات الجراحية، فإن اختيار المتلقي وإدارة المتبرعين، والحفاظ على الأعضاء المعدة للزرع، إجراءات التخدير أثناء العملية، التقدم في رعاية ما بعد العملية والعلاجات المثبطة للمناعة تزيد من نجاح البقاء على المدى الطويل بعد عملية زراعة الكبد.
شروط عملية زراعة الكبد
هناك ثلاثة مبادئ أساسية لتحديد المرضى الذين يجب إحالتهم ومن المحتمل أن يخضعوا لعملية زرع الكبد:
- يجب أن يكون لدى المتلقي مرضاً كبدياً حاداً أو مزمناً لا يمكن شفاؤه ومن المتوقع أن يكون قاتلاً بدون زرع الكبد.
- يجب أن يكون المريض بحالة تسمح للبقاء على قيد الحياة خلال فترة العملية الجراحية وما حولها.
- يجب أن يُتوقع للمريض أن يتمتع بقدر كبير من البقاء على قيد الحياة ونوعية حياة يستفيد منها بعد زرع الكبد.
ما هي أسباب عملية زرع الكبد؟
- الفشل الكبدي الحاد: يعد السبب الأكثر شيوعاً لحدوثه هو الجرعة الزائدة من أدوية الاسيتامينوفين 39%.
- خثار الشريان الكبدي في غضون 14 يوماً من زراعة الكبد.
- تشمع الكبد: المترافق بعدم المعاوضة (نزيف دوالي، اعتلال دماغي كبدي، أو استسقاء)، أو المترافق بمتلازمة الكبد الرئوي أو ارتفاع ضغط الدم الرئوي.
- الأورام الكبدية البدئية: سرطان القنوات الصفراوية النقيري وسرطان الخلايا الكبدية.
- الأمراض الاستقلابية الخلقية: التليف الكيسي المصاحب لأمراض الرئة والكبد، فرط أوكسالات البول الأولي من النوع الأول مع قصور كلوي كبير، اعتلال الأعصاب النشواني العائلي.
موانع زراعة الكبد
تشمل الموانع الأكيدة لعملية عملية زراعة الكبد كل من:
- سرطانات خبيثة فعالة خارج الكبد
- سرطان القنوات الصفراوية داخل الكبد
- سرطان الخلايا الكبدية خارج معايير ميلانو أو النقيلي
- مرض قلبي رئوي حاد
- الانتانات غير المضبوطة
- تعاطي الكحول أو المخدرات
- متلازمة نقص المناعة المكتسب (الإيدز)
- نقص الدعم الاجتماعي أو عدم الالتزام الطبي الدائم
- موانع تقنية و/أو تشريحية تحول دون إجراء عمليات زرع الكبد
تشمل الموانع المحتملة لعملية زرع الكبد كل من:
- العمر المتقدم
- خثار الوريد البابي
- عدوى فيروس نقص المناعة المكتسب
- السمنة المرضية (مؤشر كتلة الجسم BMI ≥ 40)
- ضعف الالتزام الطبي أو الدعم الاجتماعي
- الأمراض المصاحبة النفسية الفعالة (3)
تقييم حالة المتلقي قبل عملية زراعة الكبد
تنطوي عمليات زراعة الكبد على متطلبات جسدية وديناميكية دموية مشابهة لعملية جراحية كبرى، وفترة تعافي طويلة محتملة، ومخاطر تثبيت المناعة طويل الأمد، وزيادة الضغط النفسي والاجتماعي، لذا فإن عملية تقييم المتلقي ما قبل زرع الكبد مصممة لفحص المتلقي للتأكد من أنه:
- يتمتع بصحة بدنية كافية للبقاء على قيد الحياة خلال عملية زراعة الكبد والفترة المحيطة بها.
- يمكنه الالتزام بالتوصيات الطبية لضمان التطبيق الامثل للرعاية ما بعد زرع الكبد.
- لديه نظام دعم نفسي واجتماعي آمن لما بعد زرع الكبد.(3)
الفحوصات المخبرية لعملية زراعة الكبد في تركيا
الغرض الرئيسي من هذه الفحوصات قبل عملية زراعة الكبد هو تأكيد فصيلة الدم (التي يجب أن تتطابق مع عضو متبرع)، وتقييم حالة وظائف الكبد والكليتين، واستبعاد الالتهابات المصاحبة التي قد تتطلب العلاج أو يمكن أن تؤثر على الرعاية ما بعد عملية زراعة الكبد أو على نتائجها، وهذا يتضمن:
- فصيلة الدم ABO و Rh
- الاختبارات الكيميائية الأساسية
- تعداد الدم الكامل
- الإنزيمات الكبدية وعوامل التخثر
- الكالسيوم وفيتامين د
- تحليل البول
- تحري الأدوية في البول
- الاختبارات المصلية الخاصة بالتهاب الكبد A، والتهاب الكبد B، والتهاب الكبد C، وفيروس نقص المناعة البشرية، وفيروس الحماق النطاقي (VZV)، والفيروس المضخم للخلايا (CMV)، وفيروس ابيشتاين بار (EBV)، والتحري عن السل(3)
الفحوصات الشعاعية الكبدية
يجب إجراء تصوير مقطعي كافٍ للتخطيط الجراحي قبل عملية زراعة الكبد، ويعد التصوير المقطعي المحوسب ثلاثي الطور أو التصوير بالرنين المغناطيسي المعزز بالجادولينيوم الأكثر شيوعاً وقد يساعد في تحديد الحواجز التقنية المحتملة لعملية زراعة الكبد بما في ذلك خثار الوريد البابي، الدوالي حول الكبد، التشوهات التشريحية في الكبد، وعقابيل جراحات البطن السابقة.(3)
إذا تعذر الحصول على التصوير المقطعي المحوسب أو التصوير بالرنين المغناطيسي قبل عملية زراعة الكبد فقد تكون الموجات فوق الصوتية مع تقييم تدفقات دوبلر كافية، ويعد التصوير الشعاعي الكبدي أمراً بالغ الأهمية بشكل خاص للتشخيص الدقيق للمرضى المصابين بورم خبيث داخل الكبد من أجل تأكيد ترشيحهم لإجراء زرع الكبد.(3)
تقييم حالة قلب المتلقي
تهدف اختبارات القلب قبل عملية زراعة الكبد إلى التحري عن مرض الشريان التاجي و/أو أمراض الصمامات و/أو اعتلال عضلة القلب في حالة وجودها، ويمكن إجراء تدخلات علاجية محددة قبل أو أثناء عملية زراعة الكبد حسب الحاجة، وإذا كان هناك أمراض قلبية متقدمة فقد يتم إلغاء عملية زراعة الكبد.(3)
التحري عن الأورام الخبيثة
يجب إجراء فحص السرطان المناسب للعمر في جميع المرضى نظراً لأن وجود ورم خبيث خارج الكبد هو من الموانع الأكيدة لعملية زراعة الكبد، وتعتمد الفحوصات الجراة على خطر المريض، ويجب إجراؤها وفقاً للتوصيات والإرشادات المعتمدة بهذا الخصوص.(3)
اختبار كثافة العظام
يتم إجراء هذا الاختبار قبل زرع الكبد إذ تؤدي أمراض الكبد المتقدمة إلى هشاشة العظام من خلال الخمول النسبي، وقصور الغدد التناسلية، وانخفاض مستويات فيتامين د، وضعف امتصاص الكالسيوم في الأمعاء، وفي بعض المرضى الآثار المباشرة للكحول والمنشطات أو الحديد الزائد.(3)
التحري عن الأمراض الانتانية
يؤدي الخلل الوظيفي في الخلايا الكبدية إلى تعرض المرشحين لعملية زرع الكبد بشكل متزايد لخطر الإصابة بمجموعة متنوعة من الانتانات بما في ذلك التهاب الصفاق الجرثومي العفوي، ذات الرئة الاستنشاقية، الانتانات البولية، وانتانات الدم المرتبطة بالقثطرة الوريدية، يجب معالجة الانتانات الفعالة بشكل مناسب قبل زرع الكبد.(5)
حالة التلقيح والمناعة
يجب تلقيح مرضى زراعة الكبد ضد التهاب الكبد A و B إذا لم تظهر الاختبارات المصلية وجود مناعة، ويجب أن تكون لقاحات الكزاز والدفتيريا والسعال الديكي حديثة، بالإضافة إلى التلقيح ضد الأنفلونزا والمكورات الرئوية.(3)
ارتفاع ضغط الدم الرئوي
يحدث ارتفاع ضغط الدم الرئوي (وهو ارتفاع متوسط ضغط الشريان الرئوي MPAP ≤ 25 مم زئبق) بسبب وجود ارتفاع ضغط الوريد البابي ويُشار له باسم ارتفاع ضغط الدم الرئوي (POPH)، ويتم اكتشافه في 4-8% من مرشحي زرع الكبد، لا يعتبر ارتفاع ضغط الدم الرئوي الخفيف (MPAP < 35 مم زئبق) مصدر قلق كبير ولكن الارتفاع المعتدل (MPAP ≤ 35 مم زئبق) والشديد (MPAP ≤ 45 مم زئبق) يمثلان عامل تنبؤ بزيادة معدل الوفيات بعد زرع الكبد.(5)
التدخين
يعتبر التدخين متداخلاً في عدد من النتائج السلبية لدى المتلقي في زرع الكبد بما في ذلك الوفاة لأسباب قلبية وعائية وزيادة حدوث خثار الشريان الكبدي، كما ترتبط الأورام البلعوم والفم والأورام الأخرى التي تلي زرع الكبد بالتدخين ويمكن أن تؤدي إلى معدل وفيات عالي يمكن تجنبه على المدى الطويل.(5)
هناك أسباب مقنعة لحظر جميع طرق التدخين في المرشحين لعملية زرع الكبد، وتعتبر بعض برامج زراعة الأعضاء أن الإقلاع عن التدخين شرطاً لإجراء زرع الكبد وهذا يتطلب سلسلة اختبارات نيكوتين سلبية لتوثيق الإقلاع عن التدخين.(5)
خطوات عملية زرع الكبد
لعملية زراعة الكبد في تركيا أربع خطوات، وهي:
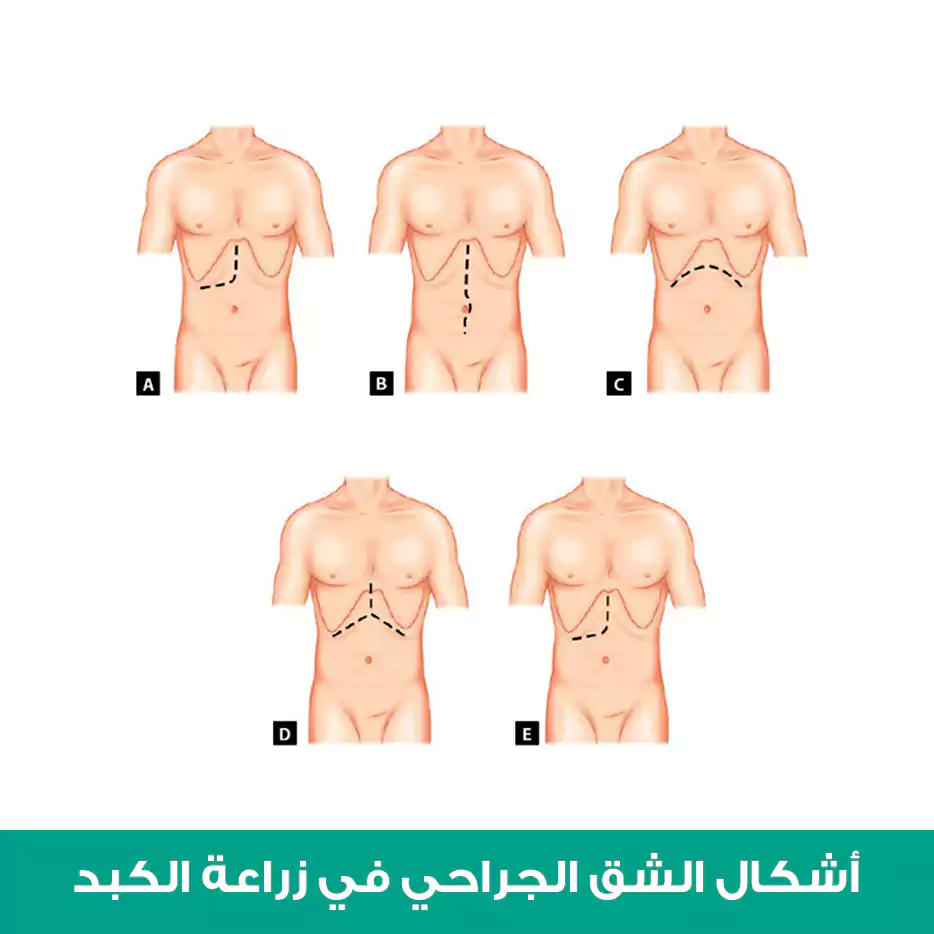
استئصال كبد المتلقي والتحضير للزرع
يُعتبر استئصال كبد المتلقي الخطوة الأولى في عملية زرع الكبد، ويمكن أن يكون إجراءً صعباً بسبب وحود علاقة تشريحية وثيقة بين الكبد والرافد الكبدي للوريد الأجوف السفلي في حالة اعتلال التخثر وارتفاع ضغط الوريد البابي.(6)
يمكن إجراء استئصال الكبد باستخدام إحدى التقنيتين التاليتين ولكن لم تثبت أي دراسة في الأدبيات الطبية تفوق إحداهما على الأخرى:
التقنية التقليدية: وفيها تتم إزالة الرافد الكبدي للوريد الأجوف السفلي الأصلي من الكبد، وتتطلب التقنية التقليدية إغلاق الوريد الأجوف بالكامل ولهذا السبب يُفضل بعض الجراحين استخدام المجازة الوريدية أثناء المرحلة اللاكبدية لتجنب عدم استقرار الدورة الدموية الناجم عن إغلاق الكلي للوريد الأجوف السفلي.(6)
تقنية على الظهر: يتم تجريد الكبد بالكامل من الوريد الأجوف السفلي، وبالتالي يتم الحفاظ على الرافد الكبدي جزئياً فقط عند الانتهاء من استئصال الكبد، وواحدة من المزايا الرئيسية لهذه التقنية هي الحفاظ على العود الوريدي خلال المرحلة اللاكبدية، لذلك تُعد هذه التقنية هي الوحيدة الممكنة عندما لا يكون الرافد الوريدي للوردي الأجوف السفلي موجوداً الطعم الكبدي.(6)
مفاغرة الوريد البابي
بعد الانتهاء من مفاغرة الوريد الأجوف السفلي يتم إجراء مفاغرة الوريد البابي بطريقة شاملة ويتم إعادة ضخ الدم إلى الكبد، ويُعد ضخ الدم أحد أهم أجزاء عملية الزرع إذ يمكن أن تترافق بعدم الاستقرار الديناميكي العميق (بطء القلب وانخفاض ضغط الدم) الناتج عن الدخول المفاجئ للبقايا السائلة الباردة والغنية بالسيتوكين في الطعم الكبدي إلى الدروان الجهازي، ولتجنب ذلك يتم غسل الطعم الكبدي بمحلول ملحي في درجة حرارة الغرفة ثم بالدم الجهازي إما من الوريد البابي أو الوريد الأجوف السفلي لغسل وتدفئة الطعم الكبدي قبل إعادة ضخ الدم فيه.(6)
مفاغرة الشريان الكبدي
تعتبر المفاغرة طرف إلى طرف بين المحور البطني في متبرع وبين الشريان الكبدي العام للمتلقي (عند نقطة التقائه بالشريان المعدي الاثني عشري) الأسلوب الأكثر شيوعاً واستخداماً لإعادة بناء الشريان الكبدي، واعتماداً على تفضيل الجراح والعوامل التشريحية قد يختلف مستوى إعادة بناء الشريان الكبدي إذ ينصب التركيز على السماح بمفاغرة واحدة بسيطة فقط في المتلقي، وتُعد مفاغرة فرع الشريان الكبدي الأيمن المنفصل للمتلقي مع جذع الشريان المعدي الاثني عشري في متبرع أسلوب إعادة البناء الأسهل والأكثر شيوعاً.(6)
مفاغرة القنوات الصفراوية
بعد مفاغرة الأوعية الدموية وإنشاء إرقاء جيد يتم استئصال المرارة وإعادة بناء القنوات الصفراوية من متبرع، والمفاغرة المفضلة هي قناة لقناة بين القنوات الصفراوية المشتركة بين المتبرع والمتلقي، وعندما يكون هناك عدم تطابق غير مقبول في حجم القناة أو أن القناة الصفراوية للمتلقي غير صالحة للاستعمال (بسبب التهاب الأقنية الصفراوية المصلب البدئي) يتم إجراء مفاغرة القناة الكبدية بالصائم.(6)
الرعاية ما بعد الجراحة في عملية زرع الكبد
يحتاج المريض الذي أجرى زرع الكبد لديه إلى رعاية خاصة، ويجب عليه اتباع توصيات الطبيب بالشكل الكامل.
مراقبة حركية الدورة الدموية بعد عملية زراعة الكبد
تعتبر مراقبة حركية الدورة الدموية بعد عملية زرع الكبد أمراً بالغ الأهمية في الرعاية ما بعد العملية، ويمكن أن تؤدي التغييرات الحادة في حركية الدورة الدموية التي لم يتم تشخيصها أو معالجتها بشكل صحيح إلى ضعف وظيفة الطعم الكبدي، إطالة مدة الإقامة في وحدة العناية المشددة، وزيادة معدل الوفيات، ويبدأ تدبير مشاكل حركية الدورة الدموية بعد العملية بفهم شامل للفيزيولوجيا المرضية المسببة.(7)
يُسبب المرض الكبدي في المرحلة النهائية عادةً ارتفاع في النتاج القلبي وانخفاض مقاومة الأوعية الدموية الجهازية، وتبدأ هذه العملية بالانعكاس بعد زرع الكبد الناجح مما يؤدي إلى انخفاض في النتاج القلبي وزيادة مقاومة الأوعية الدموية الجهازية مع تحسين الحفاظ على ضغط الدم الانقباضي.(7)
نزع أنبوب الرغامى الباكر بعد عملية زراعة الكبد
غالباً ما يكون نزع الأنبوب الرغامي التنفسي الباكر بعد زرع الكبد ممكناً بسبب تطور التقنيات الجراحية والتخديرية، وقد بدأ مفهوم نزع أنبوب الرغامى الباكر بعد العملية بجراحة القلب وتم تطبيقه على مرضى زرع الكبد في أواخر التسعينيات، ويرى المؤيدون له بأنه يقلل من خطر الإصابة بذات الرئة المرتبطة بجهاز التنفس الاصطناعي ويحسن تدفق الدم الحشوي والكبدي، كما ثبت أنه يقلل من مدة الإقامة في وحدة العناية المركزة.(7)
من الشائع ألا يتم نزع أنبوب الرغامى الباكر في غرفة العمليات لدى مرضى زرع الكبد ولا سيما الذين يعانون من أمراض رئوية موجودة مسبقاً، وهناك مجموعة من المرضى ستحتاج إلى جهاز تنفس اصطناعي لفترة طويلة مما يجعلهم عرضة لحدوث مضاعفات رئوية إضافية في فترة ما بعد العملية، لذا من الأهمية بمكان أن تمييز هؤلاء المرضى والعمل على وقايتهم من الإصابة بذات الرئة المرتبطة بجهاز التنفس الاصطناعي.(7)
التحكم بالألم بعد عملية زراعة الكبد
يُعد زرع الكبد إجراءً جراحياً كبيراً وقد يكون مصحوباً بآلام جراحية شديدة بعد العملية، وعادة ما يتم التحكم بالألم أثناء العملية وبعدها باستخدام الفنتانيل عن طريق التسريب الوريديد أو الجرعات المتقطعة، ويتم تجنب المواد المسكنة الأفيونية مثل المورفين والهيدرومورفون إن أمكن بسبب فترات نصف العمر الطويلة في حالة الفشل الكبدي.(7)
قد يحتاج بعض المرضى إلى استخدام مضخة تسكين الألم التي يتحكم بالمريض بالتوازي مع المسكنات مديدة المفعول، أو الانتقال إلى الأدوية الفموية على مدار الساعة إذا استمر الألم، ويعد التخدير فوق الجافية الصدري مفيداً للتحكم بالألم بعد جراحة البطن ولكنه لا يُستخدم روتينياً لمرضى عملية زرع الكبد.(7)
مراقبة شوارد الدم بعد عملية زراعة الكبد
يمكن أن يكون التدبير المناسب للشوارد صعباً في المرضى ما بعد زرع الكبد، وغالباً ما يعاني المرضى من العديد من اضطرابات الشوارد التي يجب مراقبتها عن كثب وتصحيحها.(7)
يعتبر فرط صوديوم الدم هو اختلاط أقل شيوعاً لدى مرضى زرع الكبد وينتج عن الفقدان الحر المفرط للمياه في المرضى الذين يستخدمون مليناً تناضحياً (مثل اللاكتولوز) لتقليل الاعتلال الدماغي الكبدي.(7)
قد يكون فرط بوتاسيوم الدم أكثر اضطرابات الشوارد خطورة بسبب التطور السريع لاضطراب نظم القلب والوفاة، وغالباً ما تكون أسباب فرط بوتاسيوم الدم بعد زرع الكبد متعددة العوامل إذ يعاني العديد من مرضى زرع الكبد إما من خلل كلوي موجود مسبقاً أو سيصابون بخلل كلوي عابر في الفترة العملية وما بعدها والذي يمكن أن يضعف آليات توازن البوتاسيوم.(7)
يتم تشخيص نقص كالسيوم الدم بكثرة في مرضى زرع الكبد، ومن المهم أن نتذكر أن هؤلاء المرضى غالباً ما يكون لديهم مستويات منخفضة من الألبومين وأن إجمالي الكالسيوم لا يعكس بالضرورة مستويات الكالسيوم الحرة لذا تكون مستويات الكالسيوم الشاردي أكثر دقة في هذه الحالة.
ويمكن أن ينتج انخفاض مستويات الكالسيوم عن عملية استخلابه باستخدام السترات المضادة للتخثر في منتجات الدم ووماد غسيل الكلى، ويجب الاشتباه بنقص كلس الدم في المريض المصاب بهبوط ضغط الدم بالرغم من الإنعاش الكافي. (7)
تتميز مستويات سكر الدم بعد زرع الكبد بأهمية كبيرة على كل من الإنذار والمضاعفات، فقد يكون نقص سكر الدم في فترة ما بعد العملية علامة على تجرثم الدم أو ضعف وظيفة الطعم الكبدي، فيما يكون ارتفاع سكر الدم (وهو أكثر شيوعا ما بعد العملية) مؤشراً لداء سكري كامن أو استجابة للتوتر أو نتيجة إعطاء الستيروئيدات.
ويرتبط ارتفاع سكر الدم الشديد (الجلوكوز> 200 ملغ/دل) بزيادة خطر رفض الطعم الكبدي وانتانات مكان العملية وزيادة معدل الوفيات.(7)
اضطرابات التخثر بعد عملية زراعة الكبد
لا يتم تحسن اضطرابات تخثر الدم فوراً بعد زرع الكبد وغالباً ما تستمر في فترة العناية المركزة بعد الجراحة، ويعود ذلك لمسببات متعددة العوامل يمكن أن تشمل انحلال الفيبرين المفرط، اعتلال تخثر الدم داخل الأوعية الدموية، تنشيط الصفيحات الدموية، احتجاز الصفيحات الدموية داخل الطعم الكبدي، ووجود التأثير المشابه للهيبارين.
كما يعاني بعض المرضى من فرط تخثر الدم بعد زرع الكبد مما يزيد من تعقيد تقييم حالة التخثر لديهم، وسبب فرط التخثر غير واضح تماماً لكن ربما ينتج عن ضعف تركيب مضاد الثرومبين بواسطة الكبد.(7)
تثبيط المناعة بعد عملية زراعة الكبد
يعتبر تثبيط المناعة بعد زرع الكبد ضرورياً لمنع رفض الطعم الكبدي، ومع ذلك يجب موازنة تثبيط المناعة مع الحفاظ على الوظائف المناعية الأخرى وخاصة منع أو تكرار الانتانات والأورام الخبيثة، ويحدث رفض الكبد المزروع بشكل أقل من الأعضاء الأخرى لذلك يمكن استخدام جرعات أقل.(7)
تُستخدم الستيروئيدات لتثبيط المناعة والتحكم بها خلال السنة الأولى بعد زرع الكبد وكذلك لعلاج نوبات الرفض الحاد، وهناك قلق من استخدام جرعات عالية من الستيروئيدات بسبب تسريع معدلات تكرار الإصابة بالتهاب الكبد الوبائي وتكرار الإصابة بسرطان الكبد والتليف الكبدي.(7)
لم يثبت أن لتجنب استخدام الستيروئيدات في تثبيط المناعة فائدةً المتلقين إيجابي فيروس التهاب الكبد الوبائي، وتشمل الآثار الجانبية الحادة الشائعة للستيروئيدات بجرعات عالية ما يلي:
- ارتفاع ضغط الدم
- عدم تحمل الغلوكوز
- الإثارة/الأرق
- خطر إصابة بالانتانات
- ضعف التئام الجروح
ويمكن التحكم في معظم هذه العلامات والأعراض لذلك نادراً ما يتم إيقاف استخدام الستيروئيدات.(7)
إعادة التأهيل بعد عملية زراعة الكبد
قد تساعد برامج إعادة التأهيل المرضى الذين يعانون من أمراض الكبد ومتلقي زرع الكبد على تحسين نوعية الحياة عن طريق زيادة قوة العضلات ومنع التعب المفرط وتعزيز القدرة الهوائية وزيادة مستوى النشاط البدني، ولهذا الغرض يجب وضع خطة محددة مناسبة للعلاج الفيزيائي بناء على احتياجات المرضى في أي مرحلة من مراحل المرض من قبل اختصاصي العلاج الفيزيائي. ويمكن تقسيم العلاج الفيزيائي بعد زرع الكبد بشكل أساسي إلى ثلاث فترات: العلاج الفيزيائي قبل الجراحة وبعد الجراحة والعلاج الفيزيائية المتأخر بعد الجراحة. (8)
يجب توضيح أسباب المشاركة في عملية إعادة التأهيل بعد زرع الكبد وموانعها بشكل جيد، فأي علامة على الرفض الحاد للكبد المزروع، النزيف الحاد، عدم توازن شوارد الدم، عدم الاستقرار الفيزيولوجي، المضاعفات العصبية الشديدة، والأمراض القلبية الوعائية الشديدة قد تؤثر بشكل أكبر على تنفيذ حركات وتمارين محددة، لذلك يجب تنفيذ إجراءات التقييم المتخصصة المعتمدة على المرحلة قبل التخطيط لبرامج العلاج الفيزيائي.(8)
يجب أن يشمل تقييم العلاج الفيزيائي لما بعد زرع الكبد قوة العضلات والقدرة على التحمل، قدرة التهوية، مستوى النشاط البدني، الاستقلالية في أنشطة الحياة اليومية ونوعية الحياة المتعلقة بالصحة، كما يجب تحديد الأمراض المصاحبة العصبية أو الاستقلابية أو العضلية الهيكلية ومستوى الألم والتعب والتدخين وعادات الكحول في سياق إجراء التقييم.(8)
مخاطر ومضاعفات عملية زراعة الكبد
لزراعة الكبد مضاعفات عديدة، لكن سنمر عليها بالتفصيل ونشرح سببها لمعرفة علاجها وطريقة تفاديها، ومن المخاطر والمضاعفات:
المشاكل التنفسية بعد عملية زراعة الكبد
يمكن أن تكون المضاعفات الرئوية شائعة جداً بعد زرع الكبد، إذ يعاني العديد من المتلقين من حالة ضعف تنفسي تتطلب رعاية تتراوح من المراقبة الدقيقة إلى التهوية الآلية لفترات طويلة، وتشمل العوامل المؤهبة ما قبل الجراحة كل من المرض الرئوي الكامن والتدخين، بالإضافة إلى ذلك فإن المرضى الذين يتم تنبيبهم قبل الجراحة معرضون لخطر احتياجات التهوية الآلية بعد الجراحة بسبب المرض الرئيسي الكامن.(7)
إن المتلازمة الكبدية الرئوية هي أحد مضاعفات تليف الكبد التي تضيف مخاوف خاصة بعد زرع الكبد إذ تؤدي إلى زيادة معدل الوفيات بعد الجراحة وخاصةً في الحالات الشديدة (PaO 2 <50 مم زئبق في هواء الغرفة)، ويعتبر نقص الأكسجة لفترات طويلة بعد زرع الكبد من المضاعفات الأكثر شيوعاً في المرضى الذين يعانون من هذه المتلازمة.(7)
المضاعفات الانتانية بعد عملية زراعة الكبد
تعتبر الانتانات السبب الرئيسي للمراضة والوفيات بعد عملية زراعة الكبد، وغالبا ما تكون الفترة المبكرة بعد الزرع (الشهر الأول) معقدة بسبب انتانات الشق الجراحي والانتانات المتعلقة بالإقامة في المستشفى بما في ذلك الانتانات البولية وذات الرئة وانتانات الدم والتهاب القولون الغشائي الكاذب.(7)
يتعرض لمرضى بعد زرع الكبد بشكل خاص لخطر الإصابة بانتانات جرثومية في الكبد والشق الجراحي تشمل الخراجات والتهاب الأقنية الصفراوية والتهاب الصفاق، لذا يجب استخدام المضادات الحيوية المعيارية وقائياً في فترة ما حول الجراحة لتقليل خطر الإصابة بالانتانات.(7)
المضاعفات الكلوية بعد عملية زراعة الكبد
إن القصور الكلوي بعد زرع الكبد أمر شائع الحدوث وتشير بعض الدراسات إلى نسبة قد تصل إلى 50% من الحالات، ويشكل النخر الأنبوبي الإقفاري الحاد السبب الأكثر شيوعاً للفشل الكلوي المبكر بعد زرع الكبد.(7)
هناك عدد من العوامل التي تساهم في زيادة خطر الإصابة بالاضطرابات الكلوية بعد زرع الكبد وهي تشمل:
- المتلازمة الكبدية الكلوية
- التهاب الكبد الوبائي C
- الداء السكري
- عدم استقرار الدورة الدموية أثناء وبعد العملية الجراحية
- نقل الدم بكميات كبيرة
- التسريب الوريدي للمقبضات الوعائية
- الانتانات
- الإجراءات الإشعاعية المتكررة
- مثبطات المناعة والمضادات الحيوية الضارة بالكلية (7)
نقص الصفيحات بعد عملية زراعة الكبد
إن انخفاض عدد الصفائح الدموية هو اضطراب شائع بعد عملية زرع الكبد، وأسباب قلة الصفيحات متنوعة ولكنها مرتبطة بانخفاض عددها في الدورة الدموية وانخفاض إنتاجها.(7)
قفي حالة تليف الكبد الشديد غالباً ما يكون هناك احتجاز كبير للصفيحات الدموية في الطحال بسبب ارتفاع ضغط دم الوريد البابي كما أن الطعم الكبدي الجديد سيحتجز الصفيحات أيضاً، وهناك انخفاض في إنتاج الصفيحات بسبب انخفاض مستويات الثرومبوبويتين في مرضى الفشل الكبدي، ويمكن أن يؤدي نقل الدم بكميات كبيرة في فترة ما بعد الجراحة إلى قلة الصفيحات بزيادة الحجم.(7)
رفض الطعم بعد عملية زراعة الكبد
هناك العديد من أنواع رفض الطعم الكبدي التي قد تحدث بعد عملية زراعة الكبد، فيمكن أن يكون رفض الطعم مفرط الحدة أو حاداً أو مزمناً أو مرض الطعم الكبدي مقابل المضيف.(7)
يمكن أن يحدث الرفض بوساطة الخلايا اللمفاوية التائية أو بوساطة الأجسام المضادة، وتستهدف العملية غالباً القنوات الصفراوية بين الفصوص والبطانة الوعائية في الوريد البابي والأوردة الكبدية وأحياناً الشريان الكبدي وفروعه.(9)
يحدث الرفض شديد الحدة بوساطة الأجسام المضادة في غضون دقائق إلى ساعات بعد عملية زرع الكبد ويحدث في 60% من حالات بسبب طعم خيفي غير متوافق مع الزمرة الدموية ABO، وفي هذه الحالة يتم اللجوء إلى فصادة البلازما، استئصال الطحال، الجسم المضاد أحادي النسيلة CD20، وريتوكسيماب لمنع حدث الرفض مفرط الحدة، ولكن غالباً ما تكون إعادة الزرع الفورية هي الخيار الوحيد.(7)
للتعرف أكثر عن دواء الريتوكسيماب يمكن مراجعة مقالة علاج سرطان لمفوما هودجكن ولا هودجكن.
يحدث الرفض الحاد بواسطة الخلايا اللمفاوية التائية ويظهر عادة في غضون أيام أو أسابيع من زرع الكبد بنسبة تتراوح بين 36-75% من الحالات، ويتميز الرفض الحاد بالتهاب وحيدات النواة وتلف الخلايا النشطة، ويمكن أن تتطور نوبات مقاومة للأدوية المضادة للرفض تؤدي إلى الرفض المزمن.(7)
يحدث الرفض بسبب مرض الطعم الكبدي مقابل المضيف في 1-2% من متلقي زرع الكبد ويرتبط بمعدل وفيات يبلغ 85%، ففي حالة زرع الأعضاء الصلبة تصبح الخلايا الليمفاوية للمانح المتبقية في اللحمة قابلة للاكتشاف في المتلقي خلال أسابيع بعد الزرع، وتتفاعل هذه الخلايا ذات الكفاءة المناعية ضد المستضدات الخلوية المختلفة الموجودة في المتلقي. وينقسم هذا الشكل من الرفض بين نمط حاد (والذي يحدث في غضون 100 يوم من الزرع) ونمط مزمن (بعد 100 يوم من الزرع).(7)
نتائج جراحة زرع الكبد
تستمر نتائج مرضى زراعة الكبد في التحسن بسبب تحسين كل من التقنيات الجراحية وأنظمة تثبيت المناعة وبسبب الإدارة الأفضل للعدوى ومضاعفات ما بعد الزرع، ومع ذلك لا يزال نقص المتبرعين يمثل التحدي الأكبر الذي يواجه قطاع زرع الكبد اليوم. (2)
ونظراً لارتفاع معدلات المراضة والوفيات المرتبطة بمرض الكبد في مراحله الأخيرة فمن الضروري أن يكون لدى الأطباء الذين يعتنون بمثل هؤلاء المرضى نظام صالح وقابل للتكرار لتقدير درجة خطورة وإنذار المرض، وسيكون هذا النظام مفيداً في تحديد أولئك الذين يحتاجون إلى عملية زرع الكبد.(2)
يُحدد العمر الفيزيولوجي وليس الزمني إمكانية قبول المريض الأكبر سنا في زرع الكبد مع الاهتمام الدقيق بالأمراض المصاحبة والحالة الوظيفية، فالنتائج الإجمالية مقبولة لدى المتلقين الذين تزيد أعمارهم عن 70 سنة على الرغم من أنها أقل جودة مقارنة بالفئات العمرية الأصغر.(4)
تم الأخذ بعين الاعتبار جودة الحياة بعد 10 سنوات و 30 سنة تالية لزرع الكبد، وكان توقع المرضى لجودة الحياة جيداً بشكل عام وكان منخفضاً فقط لدى كبار السن الذين تنخفض قدرتهم على القيام بالنشاط البدني مقارنةً بعامة السكان، كما لا يُلاحظ أي فرق من حيث جودة زرع الكبد بين المرضى الذكور والإناث، ولكن أشارت إحدى الدراسات إلى أن جودة الحياة بشكل عام كانت أعلى لدى المتلقين الذكور مقارنةً بالإناث.(4)
في النهاية نجد أن عملية زراعة الكبد من أفضل العمليات التي تجرى في تركيا لحل مشاكل الكبد بشكل نهائي، وإن تكلفة عملية زراعة الكبد في تركيا أقل بكثير من باقي الدول، ومع نفس الجودة والنتائج المتوقعة تقريبا، وإن الكثير من المرضى تحدثوا عن تجربتي مع زراعة الكبد في تركيا وكانت جميع التعليقات إيجابية ومبشرة وحتى بعد فترة طويلة من التبرع بالكبد أو زرع الكبد لديهم.
تكلفة زراعة الكبد في تركيا
تكلفة زراعة الكبد في تركيا تختلف حسب نوع المركز
حيث أن تكلفة زراعة الكبد في مشافي المدن الطبية التابعة للدولة تتراوح بين ال30 و 37 ألف دولار أمريكي.
في حين أن تكلفتها في المشافي الجامعية المتخصصة في زراعة الأعضاء تتراوح تكلفة زراعة الكبد فيها بين 45 و 55 ألف دولار أمريكي.
بينما تتراوح تكلفة زراعة الكبد في المشافي الخاصة بين ال50 و 80 ألف دولار أمريكي.
المصادر:
- Bulur A and Sevmiş M. Clinical, surgical and histopathological characteristics of liver transplant recipients: An analysis of a large sample from Turkey. Gulhane Medical Journal 2022;64:60-66.
- Ionescu, V.A, Diaconu C.C, Bungau S, Jinga V, Gheorghe G. Current Approaches in the Allocation of Liver Transplantation. J. Pers. Med. 2022;12,1661.
- Mahmod N. Selection for Liver Transplantation: Indications and Evaluation. Current Hepatology Reports 2020;19:203-212.
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Liver transplantation. Journal of Hepatology 2016;64:433-485.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alono-Coello P, et al. Evaluation for Liver Transplantation in Adults: 2013 Practice Guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. BMJ 2008;336:924-926.
- Miller C and Diago Uso T. The Liver Transplant Operation. Clinical Liver Disease 2013; 2,(4):192-196.
- Parekh K.N, et al. Postoperative Care of the Liver Transplant Recipient. Springer 2017;29:365-384.
- Yıldırım M.S, Yurdalan S.U. Physiotherapy in Liver Transplantation. InTech 2012;21:445-454.
- Zhu J.H, et al. Medical complications of liver transplantation. AME Medical Journal 2018;3:1-10.