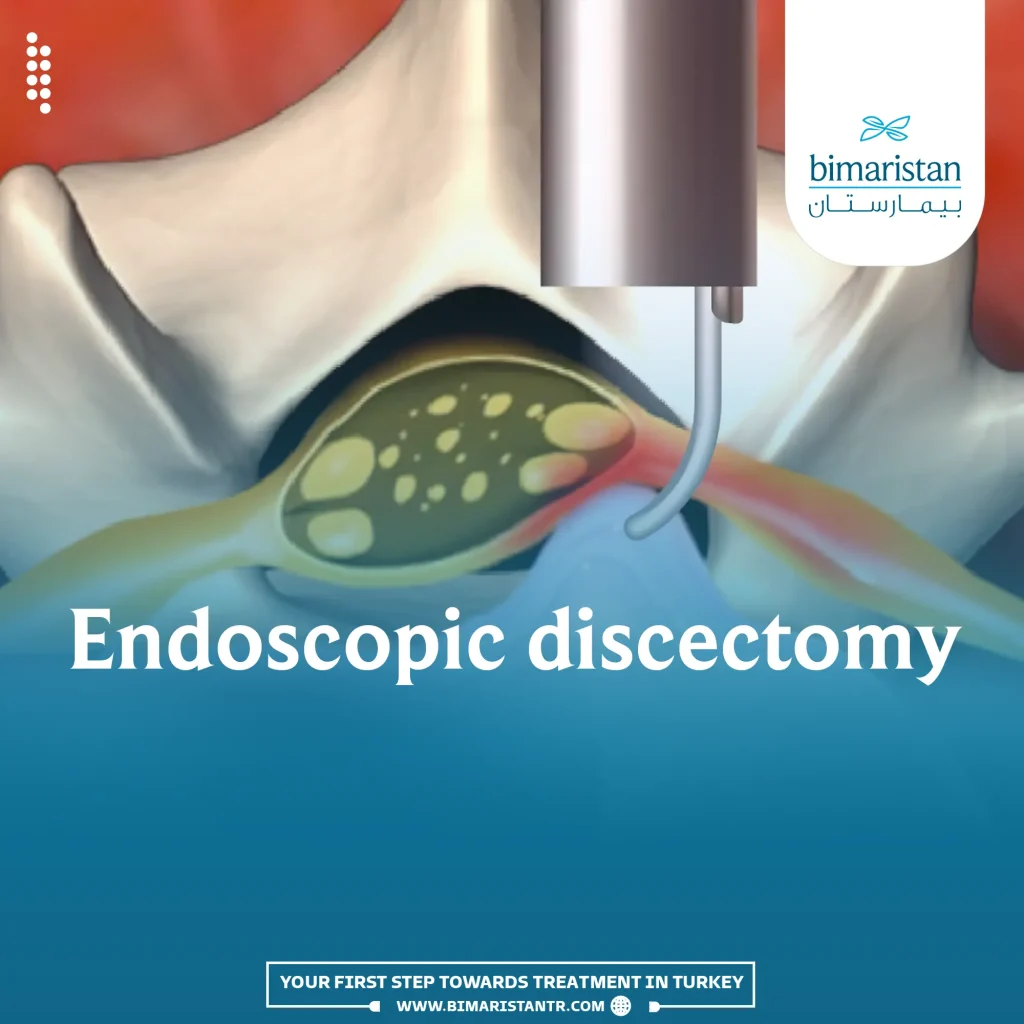
Endoscopic discectomy or Minimally invasive discectomy is a procedure that involves minimal penetration into the spinal column to remove the herniated disc nucleus that compresses the spinal nerve roots, with lower risk compared to other approaches.
Percutaneous discectomy is a relatively modern surgical procedure that involves the insertion of a tube with a camera and guiding instruments to remove the herniated disc inside the spinal canal and relieve the compressed nerve roots.
Recently, the use of minimally invasive spine surgery has started to replace traditional surgery because it leads to less patient dissatisfaction and fewer complications compared to conventional surgical procedures. Additionally, patients undergoing this procedure can enter and leave the hospital on the same day.
What is endoscopic discectomy surgery?
Minimally invasive discectomy is a type of spinal surgery that involves minimal penetration (Minimally Invasive spine surgery). In this procedure, the herniated disc, also known as the disc protrusion or herniated nucleus pulposus, is removed using an endoscope. This herniated disc causes pain due to the compression of the spinal nerve roots.
This procedure is considered one of the latest and least painful surgical methods, with a success rate exceeding 90%. It is currently one of the best available methods in Turkey for relieving pain caused by the disc.
Before discussing the procedure, it is important to understand what a disc is.
The disc (what is a herniated disc)
The spinal cord is located inside the vertebral column and exits through holes between the vertebrae. These vertebrae are connected by intervertebral discs, which relieve pressure and allow for greater mobility.
Stress on the vertebrae or heavy lifting can increase pressure on the intervertebral disc, causing a portion of it to protrude into the spaces between the vertebrae where the spinal nerves exit. This means that a part of the disc protrudes and compresses the spinal nerve roots, leading to pain, numbness, and tingling in the areas innervated by that nerve root, The so-called disc pain can occur in the neck (cervical herniated disc), back, or lumbar region (lower back).
After briefly understanding disc herniation, let’s talk about the minimally invasive discectomy procedure, which removes the herniated portion of the intervertebral disc and relieves pressure on the nerve roots.
This procedure is carried out through a small incision in the body, allowing access to the vertebral column with an endoscope through the spinal holes. The herniated disc is excised using instruments controlled by the surgeon outside the body, effectively treating the pain caused by the disc.
Indications for performing endoscopic discectomy
Firstly, it is essential to note that surgery should not be performed solely due to the presence of a disc. It is possible to manage disc-related pain through rest and pain-relieving medications when necessary.
A discectomy procedure should be performed in patients who experience symptoms that hinder their ability to perform certain tasks. These symptoms may include:
- Presence of neck, back, or limb pain after 4-6 weeks of appropriate treatment, which causes discomfort for the patient.
- Resistance to pain relief with opioids (which are strong pain relievers and can cause addiction).
- Muscle weakness in the muscles affected by the disc herniation.
- Development of advanced disc symptoms such as urinary and fecal incontinence.
Advantages of arthroscopic disc surgery
This surgical procedure has its advantages that differentiate it from the traditional disc treatment and from microscopic discectomy and also laser disc decompression, including:
- Shorter hospital stay and no need to stay for several weeks
- Lower blood loss during surgery
- Lower incidence of infections after surgery
- Faster recovery time for spinal movement and return to everyday life
- Local anesthesia is used in the disc Arthroscopy procedure, allowing the patient to interact with the doctor during the procedure, which helps the doctor ensure that the nerve root is not harmed
- It is considered the least risky among all surgical procedures for treating disc issues
How is minimally invasive discectomy surgery performed?
Before starting the endoscopic discectomy surgery, the patient is given antibiotics to reduce the risk of infection after surgery. The surgical procedure is then performed using the following steps:
Patient positioning during the procedure
The patient is placed in the prone position before starting the surgical procedure. The lateral position should be considered if the patient cannot tolerate this position due to respiratory problems or severe back pain. After achieving the appropriate position, the incision point is determined using regular anterior-posterior X-ray imaging or fluoroscopy.
Anesthesia and skin incision
The minimally invasive discectomy procedure is usually performed under local anesthesia. First, a local anesthetic (1% lidocaine) is injected to numb the skin, muscles, and nearby Intervertebral joint and to help make an incision.
Then, a 0.25% dose of lidocaine is injected into the hole between the vertebrae, reducing the dose to prevent complete nerve suppression. This allows for some sensory functions to remain, so the patient can feel pain if the surgeon gets close to the nerve roots.
Inserting the endoscope into the body
The procedure is performed under the guidance of fluoroscopic anterior-posterior imaging. Initially, a guiding wire is inserted, and the wire is inserted according to the predetermined lines. After inserting the guiding wire approximately halfway, the imaging direction changes to become lateral. The depth of insertion of the guiding wire is then checked. Afterward, the guiding wire is inserted until it touches the articular facet of the vertebrae, where the surgeon feels some resistance. The wire is then slightly withdrawn and bent perpendicularly to enter the space between the vertebrae.
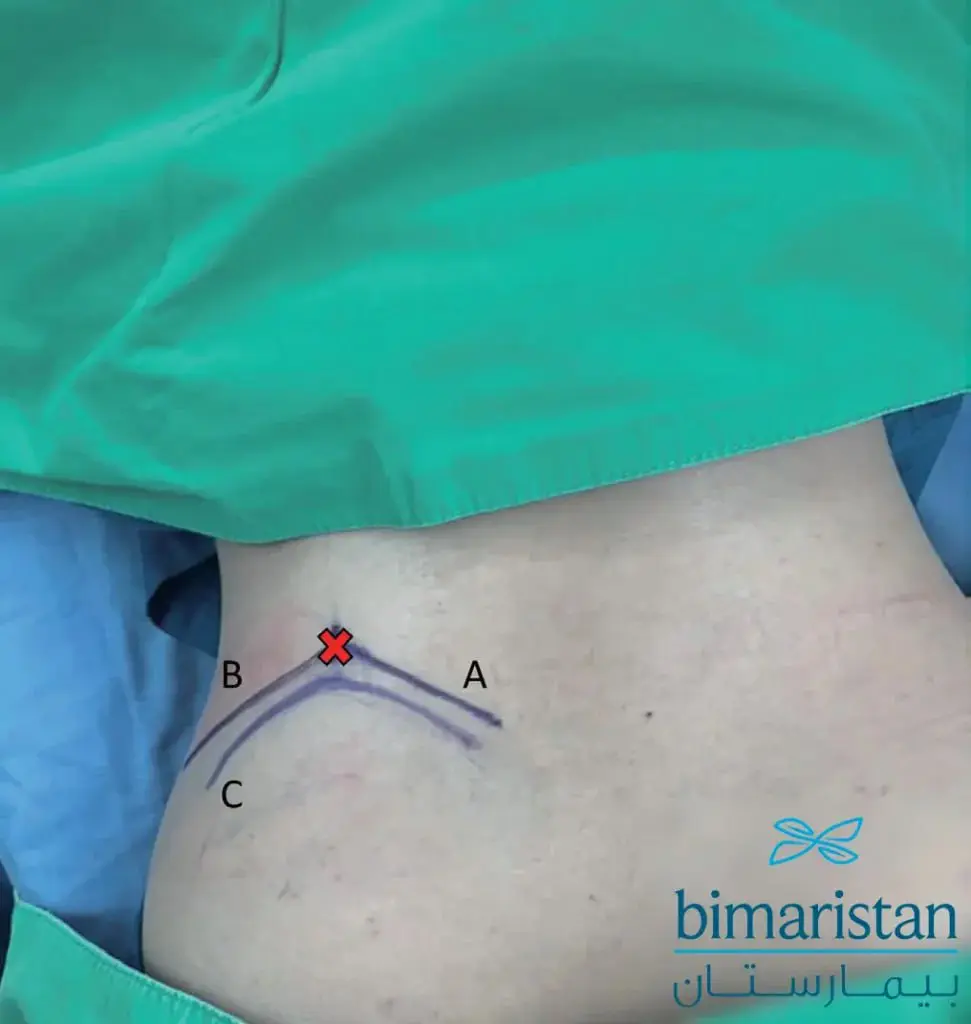
After the guiding wire is inserted, the dilator is inserted, followed by the sheath of the endoscope. Under fluoroscopic imaging, the final location of the endoscope sheath is confirmed, which is close to the base of the spinous process in lateral imaging and centered on the spinous process in anterior-posterior imaging.
Surgical procedure
In this stage, the endoscope, which contains a camera at its tip and three ports, is inserted. The largest port is called the working channel, and the two smaller ones are used for electrocautery and for the forceps.
A drill is used to drill the base of the superior articular process or the base of the vertebral peduncle. Then, electrocautery is used to coagulate the bleeding vessels, reducing blood loss.

Some vessels and ligaments in this area are then cut to facilitate freedom of movement in the area. The nerve root present in this area must be identified and protected. If the surgeon touches the nerve root, the patient will feel pain, and the surgeon will immediately move away from the root. Afterward, if a herniated disc is found in this area, it is excised.
If the disc is located more internally, the procedure continues by drilling the bone until it reaches the spinal canal. Once reached, the spinal cord sac is identified and kept away from, and the disc is located and removed.

Final check before scope removal
The doctor ensures there is no bleeding before removing the scope by using electrocautery to seal off any bleeding vessels and then withdrawing the scope and closing the incision.
Complications of minimally invasive discectomy
Minimally invasive discectomy has few complications, most of which come from the surgical procedure itself. The doctors at Bimaristan Center in Turkey are among the best in performing this procedure with precision. Some of these complications include:
- Post-operative infection
- Nerve root injury leading to paralysis
- Cerebrospinal fluid leakage due to improper bone closure
- Recurrent disc herniation after surgery
Can disc herniation recur?
The percentage of recurrent disc herniation after removal varies for several reasons, but it remains lower than in traditional surgical procedures. Some of these reasons include:
- Age
- Weight
- The type of disc present
- Degree of disc degeneration
- Higher disc height increases the risk of recurrence
The recurrence rate after a minimally invasive discectomy is estimated to be around 8.83% after the first surgery, and the rate of recurrence after a second surgery is estimated to be around 17.65%.
Tips and instructions after minimally invasive discectomy
Undergoing minimally invasive discectomy does not necessarily guarantee a full recovery and return to the pre-herniation state. Therefore, it is recommended to:
- Avoid lifting heavy weights
- Maintain proper posture while sitting in front of the TV or computer
- Engage in daily exercise
- Sleep on your sides (especially your right side) rather than on your stomach with your knees bent
- Follow a diet to lose weight if overweight
Endoscopic discectomy cost in Turkey
A minimally invasive disc surgery usually costs around $2,500 to $4,000, depending on the complexity of the procedure and the number of herniated discs that need to be removed.
In the end, minimally invasive disc surgery is a relatively modern procedure that provides a better method for removing the disc from the back with minimal scarring. Patients can often be discharged on the same day of the surgery. It is always recommended to follow some post-operative tips to minimize the risk of complications as much as possible.
References:
- Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications
- Transforaminal Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation With High Iliac Crest: Technical Note and Preliminary Series
- Medscape