يستخدم رأب الشريان السباتي وتركيب دعامة كثيراً لعلاج تضيق الشريان السباتي الشديد، فهو طريقة غير راضة توفر بديلاً جذاباً للمرضى خاصة أولئك الذين يعانون من أمراض مرافقة.
الآلية المرضية لتصلب الشرايين السباتية
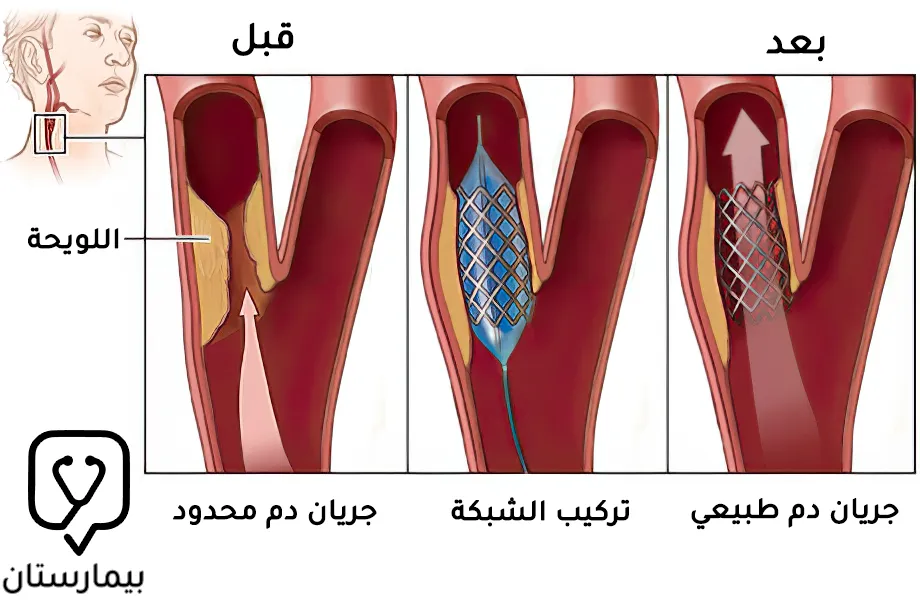
يحدث مرض الشريان السباتي كنتيجة للتصلب الذي يتشكل عند تشعب الشريان السباتي المشترك أو في منشأ الشريان السباتي الداخلي أو الخارجي، إذ تترافق ترسبات الكوليسترول في البطانة والعضلات الملساء في الشريان مع تكاثر خلوي للأنسجة العضلية الليفية والملساء المحيطة لتشكيل اللويحة العصيدية. (3)
تقلل اللويحة العصيدية الكبيرة التي تمتد إلى تجويف الشريان من تدفق الدم وتشكل سطحاً غير منتظم يكون عرضة لتكوين الخثرات، ويؤدي عدم استقرار اللويحة وتمزقها إلى تكوين خثرات انصمامية وبالتالي يؤدي إلى إصابة عصبية. ويرتبط تقرح اللويحات والخثار بأعراض عصبية بغض النظر عن درجة التضيق. (3)
خلال الفترات التعرض لنقص التروية الدموية يكون التدفق الدموي الجانبي أمراً بالغ الأهمية لتعويض تدفق الدم الدماغي ومحدداً رئيسياً لشدة نقص التروية الدماغية. وتشمل العوامل الأخرى شكل اللويحة العصيدية، ومدة نقص تدفق الدم، وخصائص الصمة الخثرية، ونشاط الأوعية الدماغية (احتياطي الأوعية الدموية الدماغية أو القدرة على توسع الأوعية). (3)
تحدد هذه التأثيرات النتيجة السريرية التي تتراوح من خفيفة (نوبة نقص تروية دماغية عابر، عجز عصبي إقفاري قابل للعكس، عمى نصفي متماثل الجانب) إلى شديدة (سكتة دماغية). وتكون المسارات الرئيسية للتدفق الجانبي هي دائرة ويليس الشريانية، وقنوات المفاغرة خارج الجمجمة، والاتصالات السحائية التي تربط مناطق البطينات بين الشرايين الرئيسية. (1)
العلاقة بين تضيق الشريان السباتي والسكتة الدماغية
تعتبر السكتة الدماغية السبب الرئيسي الثالث للوفاة في الدول الغربية ويمكن أن تسبب إعاقة دائمة، ويرتبط تصلب الشرايين السباتي بشكل مباشر بنسبة 20-30% من حالات السكتة الدماغية، لذا فإن انصمام الخثاري للأوعية الدماغية الناتج عن تصلب الشريان السباتي (الذي يسبب التضيق) يمثل مشكلة صحية هامة. (2)
تزداد نسبة حدوث السكتة الدماغية مع تقدم العمر، ففي عام 2014 كان حوالي 2.8% من عامة السكان فوق سن 18 عاماً لديهم تاريخ من السكتة الدماغية، بالإضافة إلى ذلك أصيب حوالي 795000 شخص بسكتة دماغية جديدة أو متكررة في كل عام لاحق. وكان هناك 6.5 مليون حالة وفاة بالسكتة الدماغية في جميع أنحاء العالم، كما أن 3% من الذكور و2% من الإناث أصيبوا بإعاقة بسبب السكتة الدماغية في عام 2014. (3)
وترتبط العديد من عوامل الخطر بشكل واضح بكل من تصلب الشرايين السباتية والسكتة الدماغية، ومن المهم جداً تذكر هذه العوامل كوسيلة لتقليل خطر تكرار السكتة الدماغية بعد إزالة اللويحة العصيدية من الشريان السباتي. (2)
عوامل الخطر الشائعة المرتبطة بتصلب الشرايين السباتي والسكتة الدماغية
عوامل قابل للتعديل: ارتفاع ضغط الدم، ارتفاع شحوم الدم، التدخين، السكرى، والسمنة.
عوامل غير قابل للتعديل: العمر> 80 سنة، الذكور، وجود مرض الشريان التاجي، وجود قصور القلب الاحتقاني، ووجود قصة عائلية. (2)
كشف وتشخيص تضيق الشريان السباتي
يمكن أن تظهر أعراض لتضيق الشريان السباتي وقد يكون بدون أعراض، إذ يشتكي المرضى الذين لديهم أعراض من نوبة نقص تروية دماغية عابر، بوادر سكتة دماغية أو سكتة دماغية كاملة. وتعتبر نوبة نقص التروية الدماغية العابر حدثاً عصبياً قد يستمر من عدة ثوانٍ إلى 24 ساعة، ولا يرتبط بالعجز العصبي المتبقي، ولكنه قد يكون علامة للسكتة الدماغية. (2)
يمكن الكشف على تضيق الشريان السباتي غير العرضي أثناء الفحص الفيزيائي الروتيني من خلال وجود صوت نفخة في الشريان السباتي أو أثناء الفحص بالموجات فوق الصوتية السباتية للمرضى المعرضين الخطورة العالية مثل أمراض الشريان التاجي، قصور القلب الاحتقاني، وارتفاع ضغط الدم لأن تصلب الشرايين يظهر بشكل متكرر في مواقع متعددة من نظام القلب والأوعية الدموية. (2)
إن وجود نفخة السباتي ليس معياراً موثوقاً يمكن من خلاله تشخيص تضيق الشريان السباتي بشكل مستقل، ومع ذلك يشير وجودها إلى الحاجة إلى مزيد من التحقيق عن طريق التصوير بالموجات فوق الصوتية، وتصوير الأوعية المقطعية، وتصوير الأوعية بالرنين المغناطيسي. (2)
لا تحدث جميع اللويحات العصيدية اللاعرضية في الشريان السباتي بنفس نسبة التضيق في التصوير الإشعاعي وليس لها نفس مخاطر التمزق وإحداث الانصمام الدماغي، إذ تحتوي بعض التضيقات على لويحات متقرحة (ضعيفة) غير منتظمة مع ميل مرتفع نسبياً لإحداث الانصمام والتي تتطلب عموماً تدخلاً راضاً، بينما تتميز اللويحات الملساء (المستقرة) عادة بمخاطر أقل وقد يكون من الممكن التعامل معها طبياً. (2)
إذا ظهر على المريض علامات وأعراض نوبة نقص التروية الدماغية العابرة أو السكتة الدماغية فيجب تحديد السبب، فقد تكمن أسباب الأخرى غير تضيق الشريان السباتي وراء نقص التروية الدماغي. إن معرفة جميع الأسباب أمر بالغ الأهمية ليس فقط في الحصول على تشخيص دقيق ولكن أيضاً في تقديم العلاج الأمثل. (2)
الأعراض والعلامات السريرية لتضيق الشريان السباتي
تشمل الأعراض الرئيسية لمرض الشريان السباتي: اضطرابات الرؤية، الصداع، اضطرابات الكلام، ضعف عضلات الوجه والأطراف. وتشمل العلامات التي توحي بمرض الشريان السباتي: وجود نفخة شديد الحدة عند منشأ الشريان السباتي الداخلي، زيادة في حجم ونبض الشريان الصدغي السطحي المماثل، وتغيرات في فحص الشبكية. (1)
متى يتم علاج تضيق الشريان السباتي؟
يعد المرضى الذين يعانون من تضيق الشريان السباتي بأكثر من 60% معرضون لخطر الإصابة بالسكتة الدماغية الإقفارية بنسبة تزيد عن 10% سنوياً لذلك يُوصى بعلاج هذا التضيق بإجراء إعادة فتح مكان التضيق (إعادة التروية) لتقليل مخاطر الانصمام الدماغي. ويكون تأثير إعادة التروية محدوداً في حالات تضيق الشريان السباتي الشديد غير العرضي لأن معدل تكرار السكتة الدماغية يبلغ فقط حوالي 2% سنوياً، لذلك من المفضل الحد من استخدام علاج إعادة التروية في المرضى الذين يعانون من تضيق الشريان السباتي أكبر من 80% بدون أعراض. (3)
بالإضافة إلى ذلك، يوفر علاج إعادة التروية فوائد قصوى للمرضى الذين ظهرت عليهم أعراض حديثاً إذا تم إجراؤه في غضون 14 يوماً، ولكن يمكن النظر في علاج إعادة تروية الشريان السباتي حتى في المرضى الذين لا يعانون من أعراض مع تضيق أقل حدة في الحالات التالية: وجود انسداد في الشريان السباتي المقابل، التقدم السريع للتضيق أثناء المتابعة السريرية، وجود احتشاء دماغي على تصوير الدماغ الذي لم يكن عرضياً، ووجود اللويحات الضعيفة في التصوير بالموجات فوق الصوتية. (3)
أمور يجب مراعاتها عند اختيار طريقة علاج تضيق الشريان السباتي
يُفضل استخدام رأب الشريان السباتي وتركيب دعامة لدى المرضى الذين سيواجهون صعوبة في الخضوع لعملية استئصال باطنة الشريان السباتي أو المعرضين لخطر كبير من حدوث مضاعفات أثناء الجراحة. وعلى العكس من ذلك يُفضل إجراء جراحة استئصال باطنة الشريان السباتي إذا كان من الصعب الوصول إلى موقع الآفة عبر الأوعية الدموية بالقثطرة. ومن المفيد اختيار استئصال باطنة الشريان السباتي عندما يكون زرع الدعامة صعباً أو من المتوقع حدوث مضاعفات كبيرة بما في ذلك القوس الأبهر من النوع الثالث، أو القوس البقري، أو الانحناء القريب الشديد، أو التكلس الشديد للآفة، أو الانسداد الشرايين في الفخذ، أو الانحناء الشديد للشريان الأبهر مع التكلس. (3)
العلاج بطريقة رأب الشريان السباتي وتركيب دعامة
استمرت تقنيات رأب الشريان السباتي وتركيب دعامة كعلاج داخل الأوعية الدموية في التطور حتى في الأوعية فوق الأبهر، وقد قدم رأب الشريان السباتي وتركيب دعامة علاجاً بديلاً للمرضى الذين يعانون من تضيق الشريان السباتي. كان التحسن الأكثر أهمية في نتائج أمان رأب الشريان السباتي وتركيب دعامة هو تطوير واستخدام الأجهزة التي تحمي أنسجة المخ من الصمات الخثرية، ويظهر رأب الشريان السباتي وتركيب دعامة كبديل مكافئ، بل وحتى أفضل من استئصال باطنة الشريان السباتي في معالجة تضيق الشريان السباتي لدى مرضى الجراحة عالية الخطورة وفقاً لدراسات حديثة. (2)
يعتبر توقيت إجراء رأب الشريان السباتي وتركيب دعامة بعد السكتة الدماغية موضوعاً قيد البحث، فقد يؤدي التدخل المبكر إلى حدوث نزيف في المنطقة المصابة، لذلك يُوصى به بعد 4 أسابيع على الأقل من السكتة الدماغية ما لم يكن هناك حاجة للتدخل الاسعافي. (2)
غالباً ما يتم إجراء رأب الشريان السباتي وتركيب دعامة عندما يكون استئصال باطنة الشريان السباتي صعباً من الناحية التقنية الجراحية كما هو الحال في المرضى الذين لديهم صعوبات تتعلق بتشريح العنق، تكرار حدوث التضيق بعد استئصال باطنة الشريان السباتي، أو سوابق تطبيق علاج شعاعي في منطقة العنق. وتعد التضيقات التي تكون إما مرتفعة (فوق مستوى الفك السفلي) أو منخفضة (أسفل الترقوة) أكثر قابلية للعلاج بطريقة رأب الشريان السباتي وتركيب دعامة مقارنة باستئصال باطنة الشريان السباتي. (1)
طريقة إجراء رأب الشريان السباتي وتركيب دعامة
يبدأ تحضير المريض لإجراء رأب الشريان السباتي وتركيب دعامة النموذجي بتطبيق معالجة دوائية (مثل الأسبرين وكلوبيدوجريل)، وقد تختلف الأدوية المطبقة حسب رأي الطبيب المعالج والحالة السريرية للمريض. (2)
يتم أخذ المريض إلى قسم تصوير الأوعية الدموية بالقثطرة، ويتم الدخول من الشريان الفخذي وتمرير قثطرة توجيهية إلى الشريان السباتي المصاب والمريض تحت التسكين الواعي أو التخدير العام، ثم يتم تقييم تضيق الشريان السباتي بالتصوير الوعائي الظليل. (2)
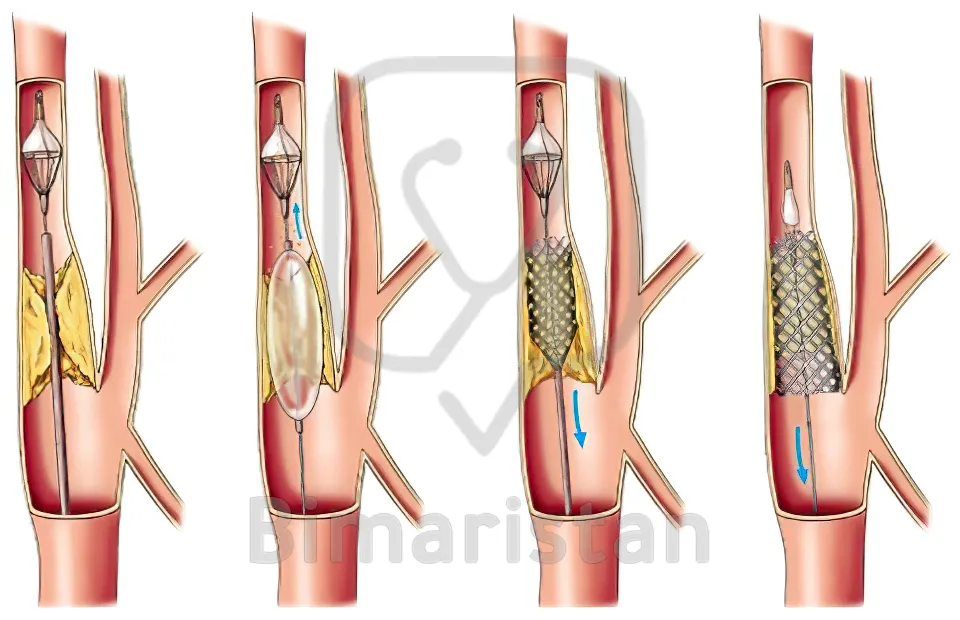
للوقاية من حدوث السكتة الدماغية الانصمامية -وهي من المضاعفات الإجرائية الرئيسية لعملية رأب الشريان السباتي وتركيب دعامة- يتم اتباع ثلاث طرق لاستخدام جهاز الحماية من الانصمام، وتشمل هذه الأجهزة الانصمام البعيد، والانصمام القريب، والترشيح (الفلترة) البعيد وهو الأكثر شيوعاً. (1)
يتم تمرير جهاز حماية الدماغ (عادة ما يكون فلتر) عبر منطقة التضيق ويتم وضعه بعيداً عن تضيق الشريان السباتي لالتقاط أي جزيئات يمكن أن تخرج من منطقة التضيق أثناء العملية، بعد ذلك يتم وضع دعامة ذاتية التمدد في منطقة تضيق الشريان السباتي. وقد يقوم الطبيب المعالج بإجراء توسيع بالبالون قبل وبعد وضع الدعامة. وفي نهاية العملية تتم إزالة الفلتر، ويتم التأكد من سالكية الدعامة وغياب الانصمام داخل الدماغ من خلال تصوير الأوعية الدموية الظليل، وعادة ما تكون مدة إجراء رأب الشريان السباتي وتركيب دعامة من 30-60 دقيقة. (2)
تتم مراقبة معدل ضربات القلب وضغط الدم بعناية أثناء إجراء رأب الشريان السباتي وتركيب دعامة، ويتم إعطاء الأتروبين لتجنب أو تخفيف بطء القلب، كما يتم علاج انخفاض ضغط الدم الحاد عن طريق الحقن الوريدي وجرعات صغيرة من مقابض الأوعية (الدوبامين أو النورأدرينالين). (4)
تتم مراقبة جميع المرضى بعد عملية رأب الشريان السباتي وتركيب دعامة من الناحية العصبية والديناميكية الدموية في وحدة العناية المركزة لمدة 12 ساعة على الأقل للتحقق من حالتهم العصبية والحفاظ على المستوى الطبيعي لمعدل ضربات القلب وضغط الدم. ويخرج المريض من المستشفى بعد 48 ساعة، ويتابع جميع المرضى العلاج المزدوج بمضادات التخثر، والعلاج الخافض الدهون، والعلاج الوقائي من ارتفاع ضغط الدم. (4)
في حالات تضيق الشريان السباتي الشديد 80%، تم إجراء التوسيع المسبق بالبالون (3-5 مم)، وبعد التوسيع يتم وضع دعامة ذاتية التمدد في موقع التضيق، ثم يتم إجراء تصوير وعائي ظليل فإذا لوحظ وجود تضيق متبقي حوالي 30% يتم إجراء توسع لاحق ببالون (5-7 مم). (4)
يمكن للجراحين استخدام أنواع مختلفة من الدعامات عند إجراء رأب الشريان السباتي وتركيب دعامة، ففي حالات تضيق الجزء القريب من الشريان السباتي المشترك من المفيد استخدام دعامة قابلة للتمدد بالبالون لإدخالها في الموضع الصحيح، كذلك فإنها مفيدة حتى في تضيق جزء قاعدة الجمجمة أو الجزء الصخري من الشريان السباتي. من جهة أخرى، يُوصى باستخدام الشبات ذاتية التمدد بدلاً من تلك القابلة للتمدد بالبالون في المواقع الأكثر شيوعاً عند تشعب الشريان السباتي أو الجزء القريب من الشريان السباتي الداخلي. (3)

رعاية المريض أثناء إجراء رأب الشريان السباتي وتركيب دعامة
يُعتبر مرض الشريان السباتي ليس عامل خطر للإصابة بالسكتة الدماغية فقط، ولكنه أيضاً يشكل مظهراً من مظاهر أمراض الأوعية الدموية الجهازية وأمراض القلب الإقفارية، فقد تم الكشف عن مرض الشريان التاجي الحاد القابل للتصحيح في 28% من المرضى الذين خضعوا لعملية رأب الشريان السباتي وتركيب دعامة في دراسة واحدة. إن التقييم قبل الجراحة لنظام القلب والأوعية الدموية يتضمن بشكل روتيني مخطط كهربية القلب والتقييم السريري الوظيفي. (1)
يجب الحفاظ على زمن التخثر النشط لأكثر من 250 ثانية عن طريق إعطاء الهيبارين، ويُنصح بإجراء تصوير الأوعية التاجية نظراً لأن أكثر من نصف المرضى الذين يخضعون لعملية رأب الشريان السباتي وتركيب دعامة يعانون من مرض الشريان التاجي بشكل كبير. (3)
عادة ما يكون الانخفاض المفاجئ في ضغط الدم أو النبض التالي لارتجاع الجيوب السباتية عابراً وبالتالي لا يوجد علاج خاص يتم تطبيقه، فمجرد تشجيع المريض على السعال سيسهل الشفاء إذا كان النبض بطيئاً جداً. ومع ذلك، يمكن أن يستمر انخفاض ضغط الدم لمدة 12-24 ساعة بعد إجراء رأب الشريان السباتي وتركيب دعامة في بعض المرضى، ففي حالة عدم وجود أعراض لديهم لا توجد حاجة إلى علاجات خاصة ما لم ينخفض ضغط الدم الانقباضي إلى أقل من 80 مم زئبق. (3)
إذا تدهورت وظيفة دماغ المريض أثناء إجراء رأب الشريان السباتي وتركيب دعامة يجب على الطبيب المعالج تقييم ما إذا كان ضغط الدم أو النبض منخفضاً جداً، وما إذا كان هناك نقص في تدفق الدم إلى مكان تضيق الشريان السباتي ويجب التحقق من اضطراب تدفق الدم أو النزيف الدماغي عن طريق إعادة التقييم صورة الدماغ. (3)
مضاعفات عملية رأب الشريان السباتي وتركيب دعامة
على الرغم من أن رأب الشريان السباتي وتركيب دعامة هو خيار علاجي غير راض متطور لا علاقة له بالجراحة المفتوحة، إلا أنه يمكن أن يكون له مضاعفات أيضاً، إذ يمكن أن تحدث بعض هذه المضاعفات أثناء الإجراء، ويمكن أن يحدث البعض الآخر بعد أسبوع. إن تقييم هذه المضاعفات مهم لمنع تفاقم الإصابة، إضافة إلى ذلك يجب تثقيف المرضى وأسرهم حول علامات وأعراض هذه المضاعفات. (2)
تبلغ نسبة حدوث المضاعفات الطبية بعد رأب الشريان السباتي وتركيب دعامة أقل من 10٪، وترتبط المضاعفات بوجود ارتفاع ضغط الدم ومرض الشريان التاجي والداء السكري والقصور الكلوي. يجب أن يركز التقييم قبل الجراحة على تحديد هذه الأمراض المرافقة وتحسين عوامل الخطر القابلة للتعديل عندما يكون ذلك ممكناً. (1)
تشمل المضاعفات المرتبطة بعملية رأب الشريان السباتي وتركيب دعامة: احتشاء دماغي، نزيف دماغي أو متلازمة فرط التروية الدموية، المضاعفات المرتبطة بموقع إدخال الدعامة، المضاعفات المتعلقة بالأجهزة الوقائية من الانصمام، المضاعفات الجهازية، والمضاعفات الموضعية في موقع بزل الفخذ. (3)
المراجع
- Erickson K.M, Cole D.J. Carotid artery disease: stenting vs endarterectomy. British Journal of Anaesthesia 2010;105: 34-49.
- Oran N.T, Oran I. Carotid Angioplasty and Stenting in Carotid Artery Stenosis: Neuroscience Nursing Implications. 2010; 42(1): 3-11.
- Park J.H, Lee J.H. Carotid Artery Stenting. Korean Circulation Journal 2018;48(2):1-17.
- Shchehlov D.V, et al. Simultaneous bilateral angioplasty and stenting for carotid stenosis – a single center experience. JOURNAL of MEDICINE and LIFE 2022;15(2): 252-257.