عملية استئصال جزء من الرئة بتقنية VATS من أحدث التقنيات الجراحية التي تجرى في تركيا من أجل علاج سرطان الرئة نظراً لكونها آمنة وذات مضاعفات قليلة بعد العملية.
تعتبر جراحة تنظير الصدر بمساعدة الفيديو Video-Assisted Thoracoscopic Surgery (VATS) إجراءً طفيف التوغل يستخدم في تركيا لإزالة الجزء المصاب من الرئة، فهو العلاج الأكثر ملائمةً لاستئصال ورم أو كتلة تضغط على الأوعية الرئوية أو المسالك الهوائية (القصبات) بالقرب من مركز الرئة.
تعتبر عملية استئصال جزء من الرئة بالمنظار من العمليات الدقيقة والمعقدة في الجراحة الصدرية نظراً لموقعها الحساس، لكنها مع ذلك ذات أهمية عالية بسبب ميزاتها التي جعلتها تتفوق على الجراحة التقليدية. تابع معنا في هذا المقال لمعرفة المزيد عن هذه العملية وكيفية إجرائها في تركيا.
أسباب استئصال جزء من الرئة
عادةً ما يكون استئصال جزء من الرئة بالمنظار هو العلاج الرئيسي للأشخاص الذين يعانون من سرطان الرئة بالمراحل الأولى، بالإضافة إلى مجموعة من الحالات يمكن أن نلجأ إلى استئصال الفص الرئوي فيها مثل:
- الأورام الحميدة؛ إذا كانت تسبب أعراضاً مزعجة أو تؤثر على وظيفة الرئة
- السل الرئوي
- الجلطات الرئوية
- النفاخ الرئوي
- خراج الرئة
- تشوهات الرئة
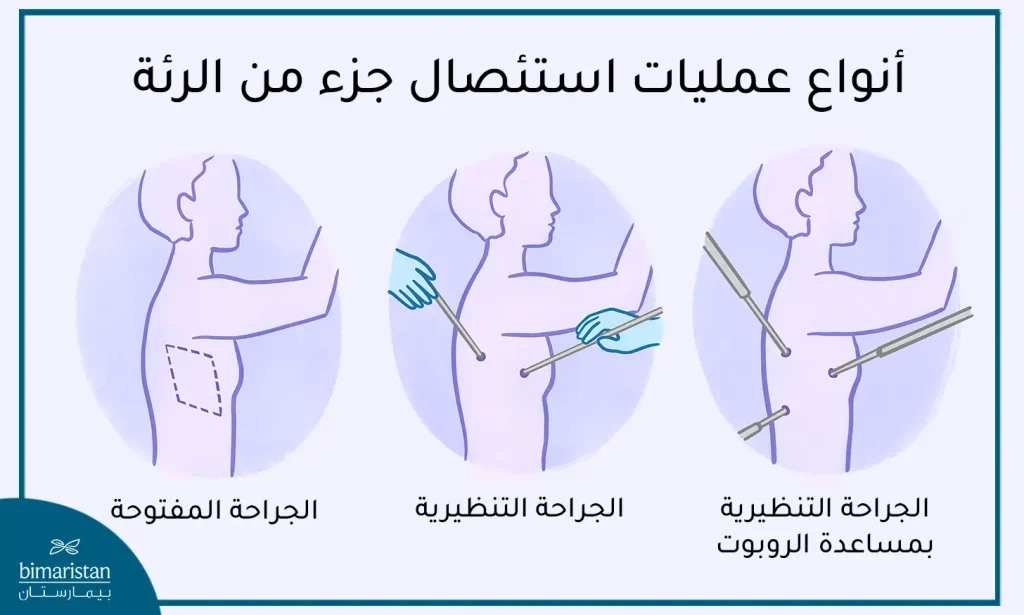
الفرق بين المنظار والجراحة المفتوحة
بعد التطور الطبي الكبير التي شهدته تركيا في العقود الأخيرة تم الاستغناء عن الجراحة المفتوحة في كثير من العمليات الصدرية وإدخال جراحة الصدر التنظيرية مكانها، وإليك أهم ميزات استئصال الفص الرئوي بالمنظار مقارنة مع الجراحة المفتوحة:
| الجراحة المفتوحة | الجراحة التنظيرية |
| تتم عبر شق جراحي واسع في الصدر مما يزيد من ضرر الأنسجة المحيطة | تُجرى الجراحة من خلال ثقب صغير في الصدر، مما يقلل ضرر الأنسجة المحيطة والنزف |
| يعاني المريض من الألم خلال فترة النقاهة بسبب التدخل الكبير على الصدر | فترة نقاهة أقل ألماً نظراً للتدخل الأقل والضرر الأقل للأنسجة |
| خطر حدوث مضاعفات أكبر | خطر حدوث مضاعفات أقل |
| تترك ندبات كبيرة وآثار جراحية واضحة على الصدر | تكون النتائج أكثر جمالية وآثار الجراحة أقل ظهوراً لأن الثقوب صغيرة |
| يستغرق الشفاء بعد الجراحة المفتوحة وقتاً أطول | الشفاء بعد الجراحة التنظيرية أسرع |
| يمكن أن تكون الجراحة المفتوحة أكثر كلفة بسبب فترة الإقامة الطويلة في المستشفى وفترة النقاهة الأطول | وسطياً تعتبر الجراحة بالمنظار ذات تكلفة أقل بسبب فترة الإقامة في المستشفى الأقصر وفترة النقاهة الأقصر – فيما عدا بعض الحالات الخاصة |
تعليمات قبل العملية
من الضروري إجراء عدد من التحاليل والفحوصات لتقييم حالة المريض وتحديد مدى تأثير الجراحة على جسمه قبل يوم من العملية، تشمل هذه التحاليل ما يلي:
- فحص الدم: لتحديد مستويات الهيموغلوبين وتعداد الكريات الحمراء والبيضاء في الدم.
- تخطيط كهربائي للقلب (ECG): لتقييم صحة القلب وتحديد فيما إذا كان المريض يعاني من أي مشاكل قلبية.
- صورة شعاعية للصدر: لتقييم حجم الورم وموقعه وتحديد مدى قابليته للاستئصال بالمنظار.
- فحص التنفس: لمعرفة قوة وكفاءة الرئتين واختبار قدرة المريض على التنفس بشكل صحيح.
- تقييم عام للصحة: يتضمن تقييم حالة المريض العامة وتاريخه الطبي والأدوية التي يتناولها.
- تحليل البول: لتحديد مستوى البروتين والسكر والكرياتينين في البول.
- اختبار تحمل الجهد: لتقييم قدرة المريض على التحمل والتعامل مع الجراحة والتخدير.
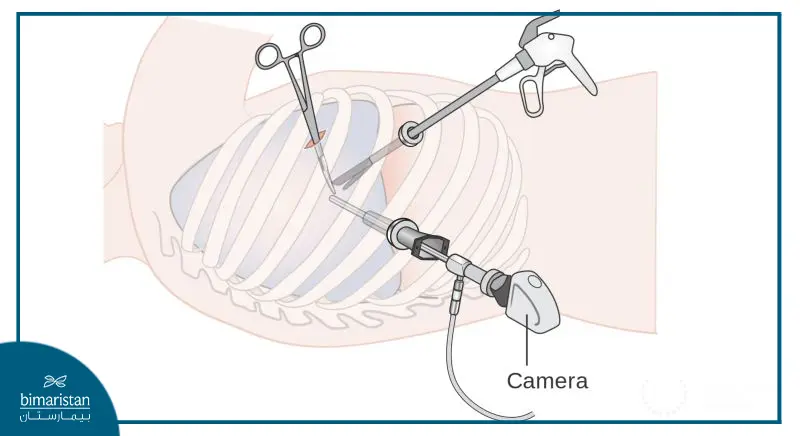
كيفية استئصال جزء من الرئة بالمنظار
تُجرى عملية استئصال فص من الرئة بالمنظار في تركيا وفق الخطوات الأساسية التالية:
- يخدر المريض تخديراً عاماً قبل بدء العمل الجراحي.
- بعد التخدير يتم إدخال أنبوب خاص في مجرى التنفس مما يتيح تهوية الرئة السليمة ريثما تجرى العملية على الرئة المصابة.
- يقوم الجراح بعمل حوالي 1-3 شقوق جلدية لإدخال المنظار وغيره من الأدوات الجراحية.
- بعد إدخال المنظار يُضخ غاز ثاني أكسيد الكربون في جوف الصدر لتوفير مساحة كافية للعمل الجراحي.
- بعد ذلك تُربط الشرايين والأوردة المتصلة بالفص الرئوي المصاب ومن ثم يقوم الجراح باستئصال ذلك الفص.
- يقوم الطبيب بإدخال أنبوب تصريف (مفجر) من أجل تفريغ الهواء داخل جوف الصدر وتخفيف الضغط فتتمدد الرئة المصابة.
- في النهاية يتم إغلاق الشقوق الجلدية وخياطتها بشكل مناسب.
إليك فيديو يوضح كيفية استئصال سرطان الرئة لمريضة عمرها 45 سنة في تركيا بتقنية VATS.
التعافي بعد العملية
يحتاج المريض إلى البقاء في المشفى 3-4 أيام بعد إجراء العملية في تركيا حتى يصبح قادراً على النهوض والعودة إلى منزله، إذا كنت من خارج تركيا فقد تحتاج إلى البقاء في الفندق لمدة يومين أو ثلاثة قبل أن تتمكن من السفر إلى موطنك الأصلي.
هناك بعض الطرق التي يجب اتباعها بعد عملية استئصال فص من الرئة لتحقيق الاستفادة المثلى من العملية وتسريع الشفاء منها:
- الحصول على قسطٍ كافٍ من الراحة وتجنب الأنشطة الشاقة لمدة تتراوح بين أسبوعين إلى شهرين.
- تجنب التدخين لمدة تتراوح بين أسبوعين إلى شهرين بعد الجراحة.
- اتباع نظام غذائي صحي وتناول الأطعمة الغنية بالبروتين والفيتامينات والمعادن لتسريع عملية الشفاء.
- متابعة العلاج الموصوف من قبل الطبيب واتباع التعليمات بشكل دقيق.
- البدء بالنشاط البدني بشكل تدريجي بعد استشارة الطبيب المعالج.
- يجب على المريض متابعة الفحوصات اللازمة لتقييم حالته بعد الجراحة والتأكد من عدم وجود أي مضاعفات.

مضاعفات استئصال فص من الرئة
بالرغم من أن عملية استئصال جزء من الرئة بالمنظار تعتبر آمنة إلّا أنها قد تشهد بعض المضاعفات المحتملة، والتي تشمل ما يلي:
- التهاب الجرح نتيجة العدوى من الأدوات المستخدمة غير المعقمة بشكل جيد، لكن بنسبة ضئيلة نوعاً ما.
- إذا لم يستخدم الجراح صارفة بعد الجراحة فقد يحدث تجمع للهواء في جوف الصدر (الاسترواح الصدري).
- قد يحدث تجمع للسوائل في الصدر (انصباب الجنب).
- قد يواجه بعض الأشخاص صعوبة في التنفس بعد الجراحة.
هذه المضاعفات نادراً ما تحدث إذا كان الجراح خبيراً باستخدام المنظار، لكن من المهم أن تبقى على اتصال مع الفريق الطبي بعد الجراحة لمتابعة أي مشاكل محتملة والحصول على العناية اللازمة.
نسبة نجاح عملية استئصال جزء من الرئة
تعتبر نتائج استئصال جزء من الرئة عادةً ممتازة، فمعظم الحالات التي أجرت هذه العملية حققت نجاحاً باهراً وتمكن المريض من العودة إلى نشاطه الطبيعي بسرعة بعد الجراحة. مع ذلك، قد تختلف نتائج الجراحة من حالة لأخرى حسب وضع المريض الصحي ونوع الجراحة المجراة.
تواصل معنا للحصول على استشارة مجانية من الطبيب المختص وفهم التفاصيل الدقيقة حول نتائج الجراحة في حالتك الخاصة.
قد تختلف نسبة نجاح عملية استئصال جزء من الرئة بالمنظار من مريض لآخر، لكنها تبلغ وسطياً حوالي 90% في تركيا (من الممكن أن ترتفع هذه النسبة في حال أجريت العملية في مركز طبي مجهز بأحدث التقنيات وتوفر طاقم طبي ذو خبرة كافية لإجراء مثل هذه العمليات).
تكلفة عملية استئصال فص من الرئة بالمنظار
يعتمد سعر عملية استئصال جزء من الرئة بالمنظار في تركيا على عدة عوامل، فهو يختلف بحسب مكان إجراء العملية والطبيب الذي يجريها وحالة المريض الصحية. على العموم، تتراوح التكلفة في تركيا ما بين 8-10 آلاف دولار أمريكي، بينما قد تصل في أوربا وأمريكا إلى أكثر من 25 ألف دولار أمريكي.
من المهم أن يتم التحدث مع الطبيب المعالج للحصول على تقدير دقيق للتكلفة بناءً على الحالة الصحية الفردية والخدمات المقدمة. ومع ذلك فإن تكاليف الجراحة في تركيا تعتبر قليلة مقارنة مع العديد من البلدان الأوربية والأمريكية مما يجعلها وجهة شهيرة للسياحة الطبية.
وختاماً، يظهر بوضوح أن عملية استئصال جزء من الرئة بالمنظار تمثل خطوة مهمة نحو الشفاء وتحسين جودة الحياة للمرضى. تقدم المستشفيات والفرق الطبية في تركيا تقنيات حديثة وخدمات متقدمة تتيح للمرضى الاستفادة من أحدث التطورات في مجال الجراحة الصدرية. سارع بالتواصل معنا للحصول على استشارة مجانية وحجز موعدك مع أفضل الأطباء في تركيا.
المصادر:


