علاج دوالي الخصية في تركيا يمكن أن يحسن بشكل كبير معايير السائل المنوي ويسمح بالحمل الطبيعي أو يقلل من الحاجة إلى المساعدة الإنجابية.
ما هي دوالي الخصيتين؟
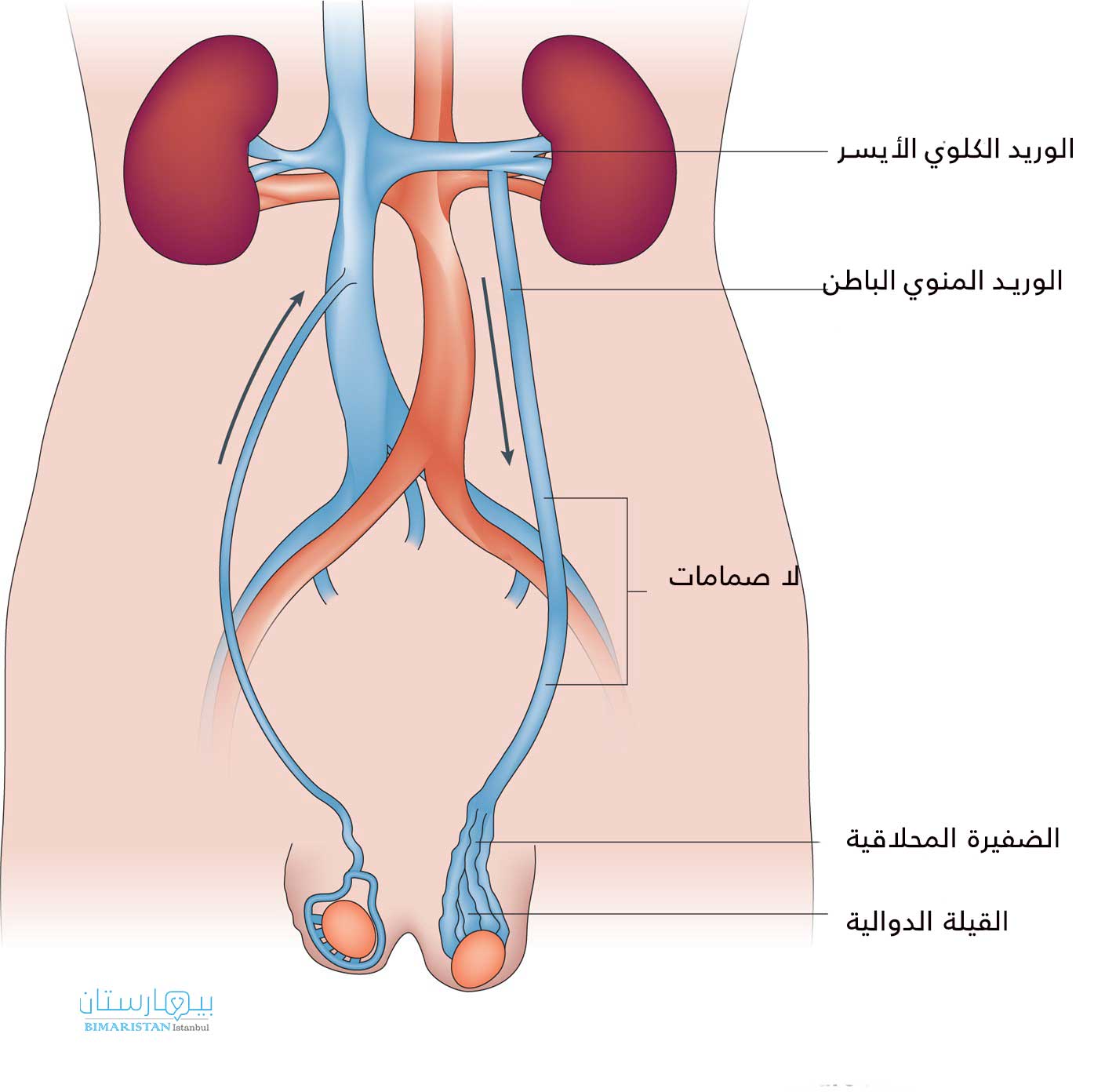
دوالي الخصية او القيلة الدوالية مصطلح يستخدم لوصف الأوردة المتوسعة بشكل غير طبيعي (تسمى “الضفيرة المحلاقية” من الأوردة) في كيس الصفن في الخصية.
كيف تتشكل دوالي الخصية؟
تنقل الأوردة في جميع أنحاء الجسم الدم من مختلف الأعضاء إلى القلب. عادة، لديهم صمامات تضمن تحرك الدم في الاتجاه الصحيح. ومع ذلك، تتشكل دوالي الخصية نتيجة حدوث خلل في عمل الصمامات في وريد الخصية.
يمكن للجاذبية أن تجعل الدم يتجمع في كيس الصفن، مما يسبب مرض دوالي الخصية. تحدث عادةً في الخصية اليسرى، ومن المحتمل أن تكون مرتبطة بمجرى الوريد الخصوي في البطن.
ما مدى شيوع دوالي الخصية؟
دوالي الخصية شائعة جدًا وليست خطيرة. في الواقع، يعاني 15٪ من الرجال البالغين من أعراض دوالي الخصية. بالنسبة للعديد من الرجال، تحدث دوالي الخصية دون أن يلاحظها أحد طوال حياتهم، أو لن تسبب أي مشاكل على الإطلاق. يعاني حوالي 20٪ من المراهقين من دوالي الخصية، لذلك من المحتمل أن يزول جزء منهم تلقائيًا.
ما هي المشاكل المرتبطة بدوالي الخصية؟
يمكن أن تسبب دوالي الخصية ثلاث مشاكل رئيسية: ضعف الخصوبة، وانخفاض إنتاج هرمون التستوستيرون من الخصية، أو عدم الراحة في كيس الصفن. لهذا السبب، لا يتم علاجهم عادة ما لم يكن هناك سبب للقلق بشأن إحدى هذه المشاكل. في بعض الحالات، يمكن أن تسبب دوالي الخصية دوالي الحبل المنوي التي تتسبب بفقد النطاف، أو النقص الكامل للحيوانات المنوية في السائل المنوي.
نظرًا لأن دوالي الخصية شائعة جدًا ولأنها عادة لا يتم اكتشافها طوال الحياة، فمن المحتمل أن حوالي 80 ٪ من الرجال المصابين بدوالي الخصية قادرون على الحمل مع شركائهم دون أي تدخل طبي. أيضًا، كما ذكرنا سابقًا، لا يعاني معظم الرجال المصابين بدوالي الخصية من مشاكل هرمونية أو إزعاج.
أحد الاعتبارات المهمة هو أن دوالي الخصية الكبيرة يبدو أن لها تأثيرات ضارة أكبر. انظر أدناه للحصول على تصنيف حجم دوالي الخصية
كيف تؤثر القيلة الدوالية على الخصية ؟
هناك العديد من النظريات، ولكن يتفق معظمها على أن إحدى الطرق هي حمل الدم الدافئ من البطن إلى أسفل باتجاه الخصية في كيس الصفن. تعمل الخصية على النحو الأمثل عند حوالي 3 درجات تحت درجة حرارة الجسم، وبالتالي يمكن أن يؤثر هذا الدم الأكثر دفئًا على قدرتها على إنتاج الحيوانات المنوية والتستوستيرون. تشمل النظريات الأخرى تأثير الكتلة على الخصية بالإضافة إلى تعريض الخصية لمواد كيميائية مختلفة من الغدة الكظرية، التي تقع بالقرب من الجزء العلوي من الوريد الخصوي.
هل لدوالي الخصية خطورة؟
دوالى الخصية ليست مهددة للحياة، ولكن نادرًا ما يمكن أن تترافق مع ظروف خطيرة. على سبيل المثال، إذا تشكلت دوالي الخصية على الجانب الأيمن وليس الجانب الأيسر، فمن المهم التأكد من عدم وجود كتلة أو أي شذوذ آخر في البطن قد يكون سببًا لها.
أيضًا، يجب أن “تقل” دوالي الخصية أو تنقص من ناحية الامتلاء عندما يكون المريض مستلقيًا لأن الجاذبية لم تعد تملأ الضفيرة الدودية في الأوردة. عندما لا تنقص دوالي الخصية، فإنها تثير القلق أيضًا من وجود انسداد في البطن مثل الكتلة أو الورم الذي يمكن أن يسبب الكتلة.
أخيرًا، يبدو أن دوالي الخصية لها دائمًا تأثيرات على إنتاج هرمون التستوستيرون. ومع ذلك، فإن العديد من الرجال المصابين بدوالي الخصية سيحافظون على مستويات مرضية من هرمون التستوستيرون طوال حياتهم دون علاج. ومع ذلك، في حالات نادرة، يمكن أن تؤدي دوالي الخصية إلى انخفاض حاد في هرمون التستوستيرون، مع المضاعفات المرتبطة به بما في ذلك المتلازمة الاستقلابية وهشاشة العظام.
ما هو نظام “الدرجات” لحجم القيلة الدوالية؟
تساعد أنظمة تصنيف دوالي الخصية في تحديد حجم دوالي الخصية، مما يساعد بعد ذلك في توجيه العلاج. تم إنشاء أنظمة مختلفة، ولكن أدناه هو المقياس الأكثر استخدامًا اليوم:
الدرجة صفر: تشاهد في الموجات فوق الصوتية، ولكن لا يمكن اكتشافه بالفحص السريري (يُسمى أيضًا “دوالي الخصية تحت الإكلينيكية”)
الدرجة I: مجسوس في الفحص السريري عندما يقوم المريض بمناورة فلسالفا (“الضغط لأسفل”)
الدرجة II: ملموس حتى بدون فلسالفا
الدرجة III: تسبب دوالي الخصية تشوهًا واضحًا في كيس الصفن.
حتى في الصفين الثاني والثالث، يمكن أن يكون هناك أحجام مختلفة يقدرها الأطباء ذوو الخبرة، ويمكن أن تساعد النتائج في تحديد ما إذا كان يجب علاج دوالي الخصية أم لا
هل يمكن أن تسبب دوالي الخصية مشاكل في وقت لاحق من الحياة؟
تشير البيانات من Johns Hopkins ومؤسسات أخرى إلى أن كلا من معايير الخصوبة ومستويات هرمون التستوستيرون يمكن أن تتأثر تدريجيًا بمرور الوقت. على سبيل المثال، يكون لـدوالي الخصية أكثر شيوعًا عند الرجال الذين أنجبوا أطفالًا سابقًا، لكنهم يواجهون حاليًا صعوبة في الحمل. أيضا، تقريبا جميع الرجال الذين خضعوا لإصلاح لـدوالي الخصية بدون جراحة يلاحظون زيادة في مستويات هرمون التستوستيرون بعد الإصلاح.
كيف يتم تشخيص دوالي الخصية؟
لا يُعتقد أن دوالي الخصية “تحت الإكلينيكية” الموجودة في الموجات فوق الصوتية ذات أهمية سريريًا، نظرًا لأنها نادرًا ما تسبب ضعف الخصية أو عدم الراحة. في حالات قليلة، قد تكتشف الموجات فوق الصوتية دوالي الخصية عندما يكون الفحص البدني صعبًا بسبب تشريح المريض، أو عندما تقود النتائج الأخرى الطبيب إلى طلب الموجات فوق الصوتية لكيس الصفن.
غالبًا ما يمكن رؤية دوالي الخصية الدوالي الوريدية التي يمكنك رؤيتها بالعين المجردة، أو يمكن أن يشعر المريض بشيء يشبه “كيس من الديدان” في كيس الصفن. الأكثر شيوعًا، مع ذلك، أن دوالي الخصية لا يتم اكتشافها إلا بعد الفحص من قبل الطبيب.
وبالتالي، فإن أفضل طريقة للكشف عن دوالي الخصية هي الفحص البدني الدقيق من قبل طبيب المسالك البولية. حتى أطباء المسالك البولية العام المخضرمين لا يكونون واثقين من التشخيص في كثير من الأحيان، لذلك إذا كان هناك أي شك، يجب على المرء الحصول على الموجات فوق الصوتية و / أو زيارة طبيب متخصص في دوالي الخصية وأمراض كيس الصفن الأخرى
متى يتم التشخيص عادة؟
عادة ما يتم العثور على دوالي الخصية بسبب أحد السيناريوهات التالية:
- الأكثر شيوعًا، في رجل بدون أعراض تمامًا يتم تقييمه من حيث العقم.
- قد يكتشف المريض أو الطبيب كتلة في كيس الصفن أثناء الفحص الروتيني.
- قد يراجع الرجل الطبيب بألم في كيس الصفن
ما نوع الألم الذي تسببه دوالي الخصية؟
بالنسبة لمعظم المرضى، لا تسبب دوالي الخصية أي إزعاج ملحوظ. ومع ذلك، يمكن أن ينتج ألم كيس الصفن الخفيف أو الشديد من دوالي الخصية. يبلغ المرضى عادةً عن إحساس “بالألم” في كيس الصفن، يرتبط عادةً بالوقوف أو النشاط لفترات طويلة. عادة ما يتم تخفيف الانزعاج عن طريق الاستلقاء (على ظهر المرء) ورفع قدمه.
قد تسبب دوالي الخصية ألمًا أكثر حدة إذا أصيبت الأوردة بالتهاب الوريد الخثاري (تخثر الدم والتهاب). يجب أن يشمل تقييم المرضى الذين يعانون من آلام كيس الصفن الموجات فوق الصوتية لكيس الصفن لاستبعاد الأمراض الأخرى، وفحص البول لاستبعاد العدوى.
يمكن النظر في إصلاح دوالي الخصية عندما لا يكون هناك سبب آخر محدد للألم وتكون صفات الألم متوافقة مع دوالي الخصية، ولكن لا يمكن أن يكون هناك ضمان بأن إصلاح دوالي الخصية سيقضي على الألم.
في العصر الحديث، يجب أيضًا مراعاة إزالة العصب عن الحبل المنوي بالجراحة المجهرية في وقت ربط دوالي الخصية في المرضى الذين يعانون من آلام كيس الصفن
دوالي الخصية والخصوبة
تم العثور على دوالي الخصية في الفحص البدني لما يقرب من ثلث الرجال الذين تم تقييمهم لفشلهم في الحمل. يتم تصنيفها حسب الحجم (انظر نظام الدرجات أعلاه) ووجودها على أحد جانبي كيس الصفن أو كلاهما. من المهم معرفة أن دوالي الخصية من جميع الأحجام قد تؤثر على الخصوبة. بالإضافة إلى ذلك، تظهر أدلة جديدة أن وظيفة الحيوانات المنوية قد تتأثر بدوالي الخصية بطرق لا يتم اكتشافها من خلال تحليل السائل المنوي.
تؤثر دوالي الخصية على جانب واحد من كيس الصفن على كلا الخصيتين فيما يتعلق بالوظيفة ودرجة حرارة الخصية. كما ذكرنا سابقًا، لا تعتبر دوالي الخصية التي لا يمكن أن يشعر بها الطبيب ولكن يتم تشخيصها عن طريق الموجات فوق الصوتية أو دراسات التصوير الأخرى مهمة سريريًا.
متى يجب القيام بإصلاحات علاجية لـدوالي الخصية؟
من المهم أن يكون لديك نهج فردي لإدارة دوالي الخصية. يتم اتخاذ قرار علاج دوالي الخصية بناءً على حجم دوالي الخصية، وأهداف خصوبة المريض، وأعراض انخفاض مستويات هرمون التستوستيرون أو عدم الراحة في كيس الصفن، واختبارات الدم مثل مستويات هرمون التستوستيرون، و / أو نتائج تحليل السائل المنوي.
أيضًا، يعد عمر وخصوبة شريك المريض من العوامل المهمة جدًا التي يجب مراعاتها عند اتخاذ قرار بشأن علاج دوالي الخصية أم لا. يجب تحديد المسار الأمثل لكل زوجين بالاشتراك مع اختصاصي الغدد الصماء الإنجابية للزوجين عندما تكون هناك اعتبارات خصوبة للإناث أيضًا. إذا لم يتم تقييم الشريكة بعد، يجب أن تخضع لاختبارات أساسية للتأكد من عدم وجود نتائج من شأنها تغيير إدارة دوالي الخصية.
هناك أدلة قوية تشير إلى أن إصلاح دوالي الخصية يحسن وظيفة الخصية وقد يمنع أي ضرر إضافي للخصية بمرور الوقت، ولكن هذا يرتبط ارتباطًا وثيقًا بحجم دوالي الخصية. وبالتالي، يجب تقييم وظيفة الخصية مباشرة عن طريق تحليل السائل المنوي، وقياس حجم الخصية، و / أو اختبارات الدم. إذا كان هناك دليل على تلف الخصية، فقد يكون إصلاح دوالي الخصية مهمًا لتحسين وظيفة الخصية و / أو منع المزيد من التدهور.
عندما يبدو أن الخصية لا تتأثر بالقيلة الدوالية، فهناك آراء متباينة حول ما إذا كان يجب علاج دوالي الخصية أم لا. إذا كنت ترغب في ربط دوالي الخصية لحماية وظيفة الخصية في المستقبل، فمن المهم إجراء مناقشة شاملة مع جراحك، والحصول على توقعات واقعية حول فرص أي فائدة قابلة للقياس، ومخاطر الآثار الجانبية من الإجراء. نحن نفضل فقط علاج مريض لأي حالة عندما تكون “نسبة المخاطرة إلى الفائدة” مواتية.
بديل العلاج هو مراقبة المرضى الذين يعانون من دوالي الخصية بمرور الوقت عن طريق فحص تحليلات السائل المنوي و / أو اختبارات الدم، والعلاج فقط إذا كان هناك دليل على أن دوالي الخصية تضعف وظيفة الخصية.
يشار إلى إصلاح دوالي الخصية في الشريك الذكر للزوجين المصابين بالعقم عندما:
- هناك دليل موضوعي على وجود عامل ذكر (مثل تحليل السائل المنوي غير الطبيعي)،
- حالة خصوبة الزوجة سليمة أو قابلة للعلاج، و
- لا توجد أسباب واضحة أخرى لعقم الذكور (مثل الانسداد أو الورم الخبيث أو الشذوذ الجيني).
كيف يتم إصلاح القيلة الدوالية ؟
هناك ثلاث فئات من الأساليب:
مع إصمام دوالي الخصية، يتم إدخال لفائف صغيرة من خلال الوريد في منطقة الفخذ وتستخدم لسد الأوردة في البطن التي تغذي دوالي الخصية. يبدو أن معدلات النجاح على المدى الطويل أقل قليلاً مقارنة بالنهج الجراحي المفتوح، ويمكن أن يستغرق العلاج أكثر من إجراء واحد. ومع ذلك، لا يوجد شق، لذلك غالبًا ما نفكر بشدة في هذا النهج للأطفال. بالإضافة إلى ذلك، يتم استخدامه أحيانًا في المرضى الذين يعانون من فشل جراحي سابق، والألم كاستطباب رئيسي للجراحة، وخصائص الجسم التي تزيد من مخاطر الجراحة مثل السمنة المرضية.
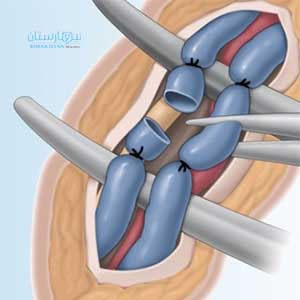
في عملية ربط دوالي الخصية بالمنظار، يتم إدخال كاميرا وأدوات صغيرة إلى البطن، حيث يتم قطع الأوردة التي تغذي دوالي الخصية. هذا الإجراء له أيضًا معدلات نجاح أقل على المدى الطويل. بالإضافة إلى ذلك، على الرغم من ندرة المضاعفات، فإنها عند حدوثها يمكن أن تكون أكثر خطورة بكثير من الطرق الأخرى. أخيرًا، يكون معدل القيلة المائية (تجمع السوائل حول الخصية) بعد الجراحة أعلى مع هذا النهج.
أخيرًا، هناك العديد من الأساليب الجراحية المفتوحة. بالنسبة لمعظم المرضى، نجري عملية ربط دوالي الخصية تحت الرباط الاربي بالجراحة المجهرية. ينتج عن هذا النهج أعلى معدلات النجاح وأقل معدلات المضاعفات، وله أقل تكلفة، ويزيل بشكل أساسي مخاطر الإصابات الخطيرة داخل البطن
كيف يتم إجراء ربط دوالي الخصية تحت الرباط الاربي بالجراحة المجهرية؟
في هذا الإجراء، يكون المريض نائمًا تحت تأثير التخدير العام. يتم إجراء شق في منطقة الفخذ السفلية وعزل الحبل المنوي. يتم تحديد جميع الأوردة التي تغذي دوالي الخصية وعزلها، مع الحفاظ على الهياكل المهمة لوظيفة الخصية.
ما هي مضاعفات دوالي الخصية التي يتم إصلاحها؟
تشمل المضاعفات المحتملة لإصلاح دوالي الخصية استمرار / تكرار دوالي الخصية والكدمات والعدوى وألم الخصية. تحدث القيلة المائية، وهي تجمع من الماء حول الخصية، في عدد قليل جدًا من الرجال. بالنسبة لأولئك المرضى الذين يخضعون لإصلاح غير جراحي، هناك خطر إضافي يتمثل في حدوث تفاعل مع عامل التباين المستخدم في الإجراء. أخيرًا، هناك خطر منخفض للغاية لفقدان الخصية.
كيف يؤثر إصلاح القيلة الدوالية بشكل إيجابي على الخصوبة؟
في 540 رجلاً مصابًا بالعقم يعانون من دوالي الخصية السريرية الملموسة والذين خضعوا لعملية استئصال دوالي الخصية بالجراحة المجهرية وتمت متابعتهم لأكثر من عام وعامين بعد الجراحة لإجراء تغييرات في جودة السائل المنوي والحمل، على التوالي:
- لوحظت زيادة بنسبة 50٪ في إجمالي عدد الحيوانات المنوية المتحركة لدى 271 مريضاً (50٪).
- تم تحقيق معدل حمل عفوي كلي بنسبة 36.6٪ بعد استئصال دوالي القيلة مع متوسط الوقت للحمل لمدة 7 أشهر (من 1 إلى 19).
- من المرشحين قبل الجراحة لإجراء / الإخصاب خارج الجسم / حقن الحيوانات المنوية داخل السيتوبلازم (أطفال الأنابيب والحقن المجهري)، أصبح 31٪ مرشحين للتلقيح داخل الرحم (IUI).
- من بين جميع المرشحين لإجراء IUI اكتسب نسبة 42٪ إمكانية الحمل التلقائي.
- استئصال القيلة الدوالية بالجراحة المجهرية لديه إمكانات كبيرة ليس فقط لتفادي الحاجة إلى التكنولوجيا الإنجابية المساعدة، ولكن أيضًا لتقليل أو تغيير مستوى التكنولوجيا الإنجابية المساعدة اللازمة لتجاوز عقم عامل الذكور.
هذا يعني أن إصلاح دوالي الخصية المهمة سريريًا يمكن أن يحسن بشكل كبير معايير السائل المنوي ويسمح بالحمل الطبيعي أو يقلل من الحاجة إلى المساعدة الإنجابية.