يعد السلس البولي من أشيع المشاكل التي تصيب كبار السن وتؤثر على حياتهم وأنشطتهم، تعرّف في هذه المقالة على أهم أسباب سلس البول عند الرجال وطرق علاجه في تركيا.
سلس البول عند الرجال
يعرف السلس البولي urinary incontinence بأنه فقدان قدرة المثانة على تخزين البول بشكل جيد مما يؤدي إلى تسرب البول عبر الإحليل بشكل غير مقصود.
لا يعتبر السلس incontinence مرضاً بحد ذاته وإنما هو عرض لمشكلة في السبيل البولي.
يعتبر سلس البول عند الرجال مشكلة شائعة ومحرجة، تشير الإحصائيات إلى أن 3.4 مليون رجل في الولايات المتحدة الأمريكية يعانون من السلس البولي ويواجهون صعوبات في التأقلم مع المجتمع، كما تشير دراسة سويدية إلى أن نسبة شيوع سلس البول عند الرجال تقدر بـ 22.6% مقارنة مع 49.0% عند النساء.
هنالك عدة أنواع لسلس البول عند الرجال والنساء، بعضها أشيع عند الرجال أكثر منه عند النساء، يزداد شيوع هذه الحالة مع التقدم بالعمر لكنها ليست حتمية وتكون قابلة للعلاج عادة.
يحتاج سلس البول إلى معالجة طبية جدية عندما يؤثر على الأنشطة اليومية ويعيق صاحبه من أداء عمله، قد تكفي بعض التغيرات البسيطة في السلوكيات اليومية والنظام الغذائي لعلاج أعراض سلس البول وقد يتطلب إجراءات طبية خاصة من أجل علاج عدم التحكم في البول عند الرجال.
أعراض سلس البول
يعتبر السلس البولي urinary incontinence بحد ذاته عرضاً لمشكلة أخرى أو مرض مستبطن، قد يكون سلس البول قصير الأمد يشير إلى أذية مرضية أو علاجية وقد يكون طويل الأمد (مزمن) يتميز ببدايته التدريجية.
هنالك أنواع من السلس البولي قد تسبب أعراضاً مميزة إضافة إلى التسرب البولي اللاإرادي، تتضمن أنواع سلس البول مزمن:
- السلس الجهدي: يحدث عندما يكون الضغط الخارجي على المثانة الضعيفة هو السبب في تسرّب البول، قد يأتي الضغط الخارجي من السعال أو العطاس أو الضحك أو حمل الأشياء الثقيلة.
- السلس الإلحاحي: يحدث عندما تشعر برغبة شديدة ومفاجئة في التبول بشكل متكرر، قد لا تتمكن من الوصول إلى الحمام في الوقت المناسب فتتقلص المثانة من تلقاء نفسها وتؤدي إلى تسرب لاإرادي للبول.
- السلس المختلط: يجمع هذا النوع من السلس بين سلس البول الجهدي وسلس البول الإلحاحي.
- السلس بفرط الإفاضة: يتصف بوجود رغبة في التبول إلا أنك لا تستطيع التبول إلا بكمية قليلة مما يؤدي إلى عدم إفراغ المثانة وتسرب البول فيما بعد، يعود ذلك إلى وجود انسداد أو إعاقة في مخرج المثانة كما في تضخم البروستاتا.
- السلس الوظيفي: ينجم هذا النوع من سلس البول عن وجود خلل جسمي أو عقلي يمنعك من الوصول إلى الحمام في الوقت المناسب.
لقد أثبتت الدراسات أن واحد من كل خمس رجال لديهم اعراض سلس البول يطلبون العناية الطبية فقط، وأنه على الرغم من توافر العلاجات المناسبة إلا أن نسبة الرجال الذين يطلبون العناية تقدر بنصف نسبة النساء المصابات بسلس البول اللواتي يطلبن العناية.
أسباب سلس البول عند الرجال
تمتلك الأنواع المختلفة من السلس البولي urinary incontinence أسباباً مختلفة، قد تؤدي بعض العادات اليومية أو الأمراض المستبطنة أو المشاكل الجسمية إلى حدوث سلس البول عند الرجال، تتضمن أشيع أسباب عدم التحكم في البول عند الرجال:
المشاكل التي تتعلق بالبروستات
تعد مشاكل البروستات والعمليات اللازمة لعلاجها أشيع سبب لحدوث سلس البول عند الرجال، حيث يزداد حجم البروستاتا مع التقدم بالعمر.
تتضخم البروستاتا غالباً بسبب فرط تنسج البروستات الحميد عند متوسطي العمر، وربما تكون الضخامة ناتجة عن سرطان البروستاتا (أشيع سرطان عند الرجال) خصوصاً في الأعمار المتقدمة.
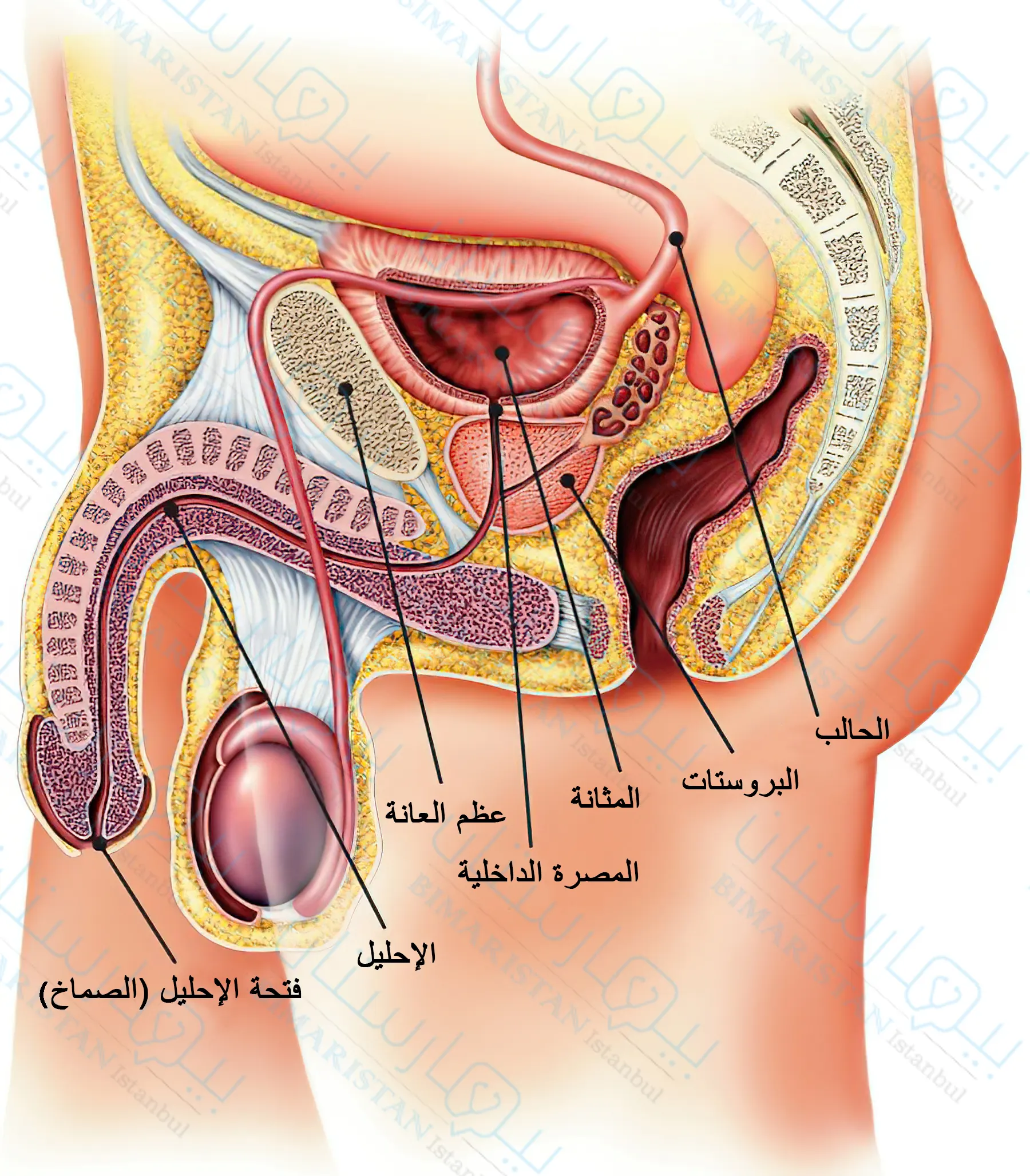
عندما تتضخم البروستاتا تضغط على الإحليل فتؤثر بذلك على تدفق البول وتسبب ضعف رشق البول وتعدد بيلات وقد يحدث تسرّب البول وسلس بفرط الإفاضة.
يمكن أن يكون سبب عدم التحكم في البول عند الرجال وجود أذية أو ضعف في المصرة البولية بعد عملية استئصال البروستاتا فينتج سلس جهدي يتحرض عند زيادة الضغط على المثانة.
قد يكون سلس البول بعد جراحة البروستاتا مؤقتاً، لكن في حالات أخرى يستمر سلس البول ويتطلب عناية خاصة لعلاجه.
في حال وجود تضخم في البروستاتا فإننا نصح بعلاجها بواسطة التخثير عن طريق القسطرة أو بواسطة الليزر لمنع حدوث سلس في البول مستقبلاً.
الحالات التي تؤدي إلى أذية عصبية
تقوم الأعصاب بتنبيه الشخص عندما تمتلئ مثانته وتتحكم بعمل عضلة المثانة والمصرات البولية، لذلك يتطلب التبول الطبيعي سلامة كل من الأعصاب والعضلات وإن أي مرض أو أذية فيهما قد ينتج عنه مشاكل بولية.
تتضمن الأذيات العصبية:
- داء باركنسون
- داء الزهايمر
- الاحتشاء الدماغي
- السكري
- التصلب المتعدد
- الديسك أو فتق النواة اللبية
- إصابات النخاع الشوكي
- الخرف
- قطع الأعصاب التي تغذي المثانة والمصرات أثناء الجراحة (خاصة جراحة البروستاتا)
تتنوع المشاكل البولية التي ترافق الأذية العصبية بحسب مكان الأذية، فقد يحدث سلس إلحاحي أو سلس بفرط الإفاضة، وقد تنتج حالة تسمى المثانة مفرطة الفعالية؛ أي أن المثانة تتقلص لاإرادياً ولا تعود تخضع لسيطرة المريض.
تحدث مع طبيبك لمعرفة أسبابه العصبية بدقة.
كمية ونوعية السوائل التي يتم شربها
يمكن لأنواع معينة من المشروبات أن تجهد الجهاز البولي، تمتلك القهوة والكحول تأثيراً مدراً للبول على سبيل مثال وإن الحد من شربهما قد يساعد على التحكم بالمثانة بشكل أفضل.
على الرغم من ذلك فإن شرب السوائل يعتبر ضرورياً للمحافظة على صحة الجهاز البولي، لكن بشرط عدم الإفراط في إدخال السوائل إلى الجسم لأن ذلك يفاقم مشاكل السيطرة على المثانة.
الحالة الوزنية
يمكن لزيادة الوزن أن تفاقم من مشكلة سلس البول، عندما تتراكم الدهون في الجسم ستشعر المثانة بمزيد من الضغط مما يجعل البدين يشعر بحاجة إلى التبول عدداً أكبر من المرات ولا يستطيع حبس بوله لفترات طويلة.
طرق تشخيص سلس البول عند الرجال في تركيا
سيقوم الطبيب بسؤالك عن سوابقك المرضية والأعراض التي تشتكي منها حالياً، كما سيقوم بفحصك سريرياً مع إجراء بعض الاختبارات على البول، عادة ما يكون ذلك كافية لمساعدة الطبيب على الوصول إلى التشخيص ومعرفة نوع السلس لديك وسببه.
قد يطلب منك الطبيب تسجيل كمية السوائل التي تشربها ووقت وعدد مرات التبول وتقدير كمية البول في كل مرة لعدة أيام، ومن المهم أن تذكر للطبيب فيما إذا كنت تشعر بإلحاح بولي أو حدث سلس ولم تتمكن من الوصول إلى الحمام في الوقت المناسب.
قد يحتاج الطبيب إلى قياس قوة رشق البول عبر أجهزة خاصة تقيس التدفق الأعظمي للبول ومعدل الجريان الوسطي ثم حساب كمية التبول والكمية التي بقيت في المثانة بعد التبول (الثمالة البولية)، وذلك لتأكيد نوع السلس لديك والكشف عن وجود انسداد في السبيل البولي أيضاً.
علاج سلس البول عند الرجال في تركيا
يعتمد علاج سلاسة البول عند الرجال بشكل أساسي على سبب السلس لديهم ونوعه، قد يتضمن العلاج إجراء تغييرات في الحياة اليومية أو تناول أدوية أو كليهما معاً، في بعض الحالات الأخرى يُنصح بإجراء أساليب حديثة أو عمليات جراحية من أجل علاج سلاسة البول عند الرجال.
التغييرات السلوكية في الحياة اليومية لـ علاج سلس البول للرجال
قد ينصحك الطبيب بما يلي:
- اذهب إلى الحمام عدة مرات في اليوم ولا تحبس البول لفترات طويلة، اختر لبس الثياب التي يمكن خلعها بسهولة ومهّد الطريق إلى الحمام لكي تستطيع الوصول إليه بسرعة قبل تسرب البول.
- شرب السوائل بكمية كافية واتباع نظام غذائي صحي سيساعد على تخفيف الوزن واستعادة التحكم بالمثانة، اختر المشروبات الطبيعية الصحية وابتعد عن المشروبات الغازية والكحول والقهوة والشاي.
- قم بتدريب المثانة عبر حبس البول ومنعه من التسرب بعد الشعور بإلحاح بولي، حاول البدء بعشر دقائق ثم قم بزيادة المدة تدريجياً، سيساعدك ذلك على إطالة الفترة ما بين الشعور برغبة بالتبول وتسرب البول كي تتمكن من الوصول الحمام قبل أن تبلل ثيابك.
- قد تساعد تمارين كيجل Kegel exercises على تقوية عضلات أرضية الحوض التي تساعد على استمساك البول، وتعتبر هذه الطريقة فعالة في السلس الجهدي بشكل خاص إلا أنها قد تكون ذات فائدة في السلس الإلحاحي.
- استخدم مفكرة لتسجيل عمليات التبول اليومية والأعراض التي ترافق التبول وسلس البول في حال حدوثه، قيامك بذلك سيساعد الطبيب على اختيار أفضل علاج لسلس البول في حال لم تكن التغييرات في العادات اليومية كافية لمعالجة السلس.
العلاج الدوائي لسلس البول
غالباً لا تفييد العلاجات الدوائية في علاج السلس الجهدي، بالمقابل يوجد العديد من الأدوية التي تستخدم في علاج السلس الإلحاحي.
تتضمن ادوية سلس البول عند الرجال ما يلي:
- مضادات الكولين: تشمل هذه الفئة الدوائية العديد من الأدوية مثل oxybutynin وتقوم بتهدئة المثانة مفرطة الفعالية ويمكن أن تكون مفيدة في السلس الإلحاحي.
- ميرابغرون Mirabegron: يقوم هذا الدواء بإرخاء عضلة المثانة فتزداد قدرتها على استيعاب البول وتزداد كمية التبول مما يساعد على تفريغ المثانة بشكل أفضل، يستخدم هذا الدواء في علاج سلس البول الإلحاحي بشكل خاص.
- حاصرات ألفا مثل tamsulosin: تقوم بإرخاء عضلات عنق المثانة والألياف العضلية في البروستات مما يسهل من تفريغ المثانة، تستخدم حاصرات ألفا في علاج السلس الإلحاحي والسلس بفرط الإفاضة عند الرجال الذين لديهم بروستات متضخمة.
ننصح بعدم اتباع الأشخاص الذين يتحدثون عن علاج سلس البول عند الرجال بالأعشابلأنه إلى الآن لا يوجد أي دليل واحد على فعاليتاها.
تقنيات حديثة لعلاج سلس البول عند الرجال في تركيا
وهي علاجات غير جراحية مفيدة في علاج أنواع السلس البولي، تتضمن:
- التنبيه الكهربائي لعلاج سلس البول للرجال
يتم التنبيه الكهربائي عبر إلكترودات توضع مؤقتاً في المستقيم لتقوية عضلات أرضية الحوض، قد يكون التنبيه اللطيف فعالاً في علاج السلس الجهدي والسلس الإلحاحي، يجب تكرار هذا الإجراء عدة مرات على مدى أشهر.
- المواد المضخمة Bulking agents
وهو إجراء تنظيري تُحقن فيه مواد صنعية تحت بطانة الإحليل لتضييق اللمعة والمساعدة على استمساك البول ومنع تسربه لذلك يستخدم في علاج السلس الجهدي.
يمكن تنفيذ هذا الإجراء في العيادات الخارجية ولا يتطلب أية شقوق جراحية إلا أن نجاحه محدود مقارنة مع الإجراءات الأخرى الأكثر بَضْعاً كالجراحة، علماً أنه يمكن تكراره أكثر من مرة.
- الذيفان الوشيقي من النمط A (البوتوكس)
يمكن حقنه داخل عضلة المثانة للمساعدة في إرخائها، قد يكون هذا الإجراء مفيداً للذين يعانون من المثانة مفرطة الفعالية أو السلس الإلحاحي وغالباً ما يلجأ إليه عند فشل العلاجات الأخرى.
- تنبيه الأعصاب العجزية Sacral nerve stimulation
يستطب تنبيه الأعصاب العجزية الذي يعرف أيضاً بالتعديل العصبي sacral neuromodulation عندما يكون السلس الإلحاحي ناتجاً عن التقلص المتكرر أكثر من اللازم لعضلة المثانة (المثانة العصبية).
تقوم الأعصاب العجزية بالتحكم بتقلص عضلة المثانة، فعند تنبيه هذه الأعصاب بنبضات كهربائية معتدلة يتأثر تقلص هذه العضلة مما يمنع سلس البول.
يُزرع في هذا الإجراء جهاز صغير (محول عصبي) تحت جلد أسفل الظهر قرب موقع الأعصاب العجزية، يقوم الجهاز بإرسال الإشارات الكهربائي إلى هذه الأعصاب.
علاج سلس البول عند الرجال جراحياً في تركيا
في حال فشل الإجراءات الأخرى غير الباضعة يمكن اللجوء إلى الجراحة كحل أخير، تتضمن الإجراءات الجراحية لعلاج سلس البول عند الرجال نوعين من العمليات، وقد أظهرت الدراسات أن كلا الإجرائين قد ساهم في تحسين اعراض سلس البول:
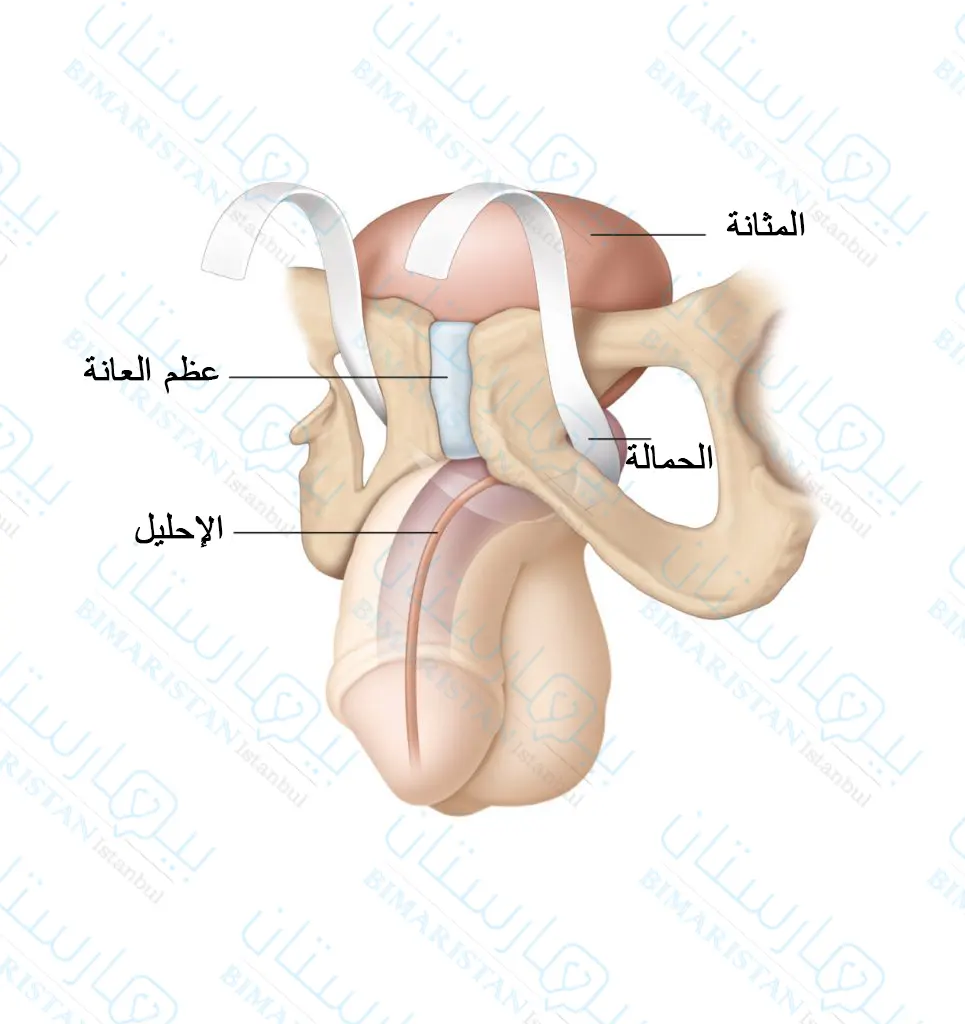
علاج عدم التحكم في البول عند الرجال بواسطة الحمالة الذكرية Male sling
يقوم الطبيب باستخدام نسيج أو مادة صنعية لإنشاء عروة تحيط بالإحليل وعنق المثانة مما يساعد على إبقاء الإحليل مغلقاً أثناء السعال أو العطاس.
تؤمن الحمالة الذكرية القدرة على استمساك البول بشكل أكبر عند المرضى الذين يشتكون من سلس جهدي خفيف، علماً أنه يمكن إجراء هذه التقنية طفيفة التوغل والخروج من المشفى في نفس اليوم بالنسبة لمعظم المرضى.
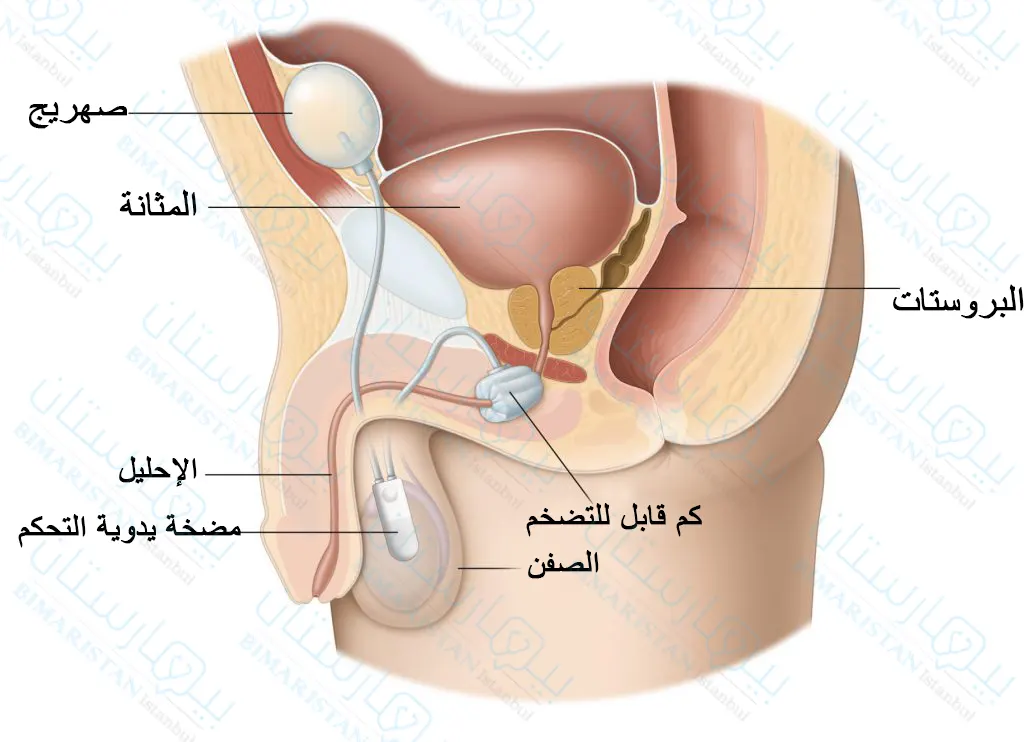
المصرة البولية الصنعية Artificial urinary sphincter
تعد عملية زرع المصرة الصنعية العلاج الذهبي للسلس الجهدي عند الرجال، وهي فعالة في علاج السلس المعتدل إلى الشديد.
تزرع في هذه العملية حلقة صغيرة مملوءة بالسائل تدعى الكف حول عنق المثانة من أجل إبقاء المصرة البولية مغلقة لحين الحاجة إلى التبول.
عند التبول يقوم المريض بالضغط على صمام مضخة مزروعة تحت جلد الصفن لإفراغ الحلقة من السائل والسماح لبوله بالخروج من المثانة، ينتقل السائل ويتجمع في صهريج مؤقتاً ريثما ينتهي المريض من التبول ثم يعود ليملأ الحلقة ويغلق المصرة من جديد.
أدوات ومنتجات للسلس البولي عند الرجال
عند فشل جميع العلاجات السابقة في إيقاف سلس البول يمكنك استخدام منتجات خاصة للتخفيف من الانزعاج والإحراج المرافقين لتسرب البول، تتضمن:
- الحفاضات والسراويل الواقية وهي ملابس داخلية مصممة خصيصاً لامتصاص البول المتسرب من السلس، ومن الملاحظ أن هذا المنتج لا يوقف السلس ولكنه يساعد في التعايش معه ومنع وصول البول إلى الملابس الخارجية.
- القساطر: تساعد القساطر على إفراغ المثانة كلياً لذلك ينصح الأطباء باستخدام هذه الأداة في حال وجود ثمالة بولية بعد التبول، حيث يُدخل أنبوب مرن عبر الإحليل عدة مرات في يومياً لتصريف البول من المثانة، يجب أن يكون المريض واعياً وملماً بطريقة تطبيق القسطرة من أجل الاستخدام الآمن.