تميل أعراض التهاب البنكرياس الحاد لتظهر دون سابق إنذار فقد تشعر فجأة بألم شديد في الجزء العلوي من البطن، بينما تكون أعراض الالتهاب المزمن مخادعة وتستمر فترة أطول.
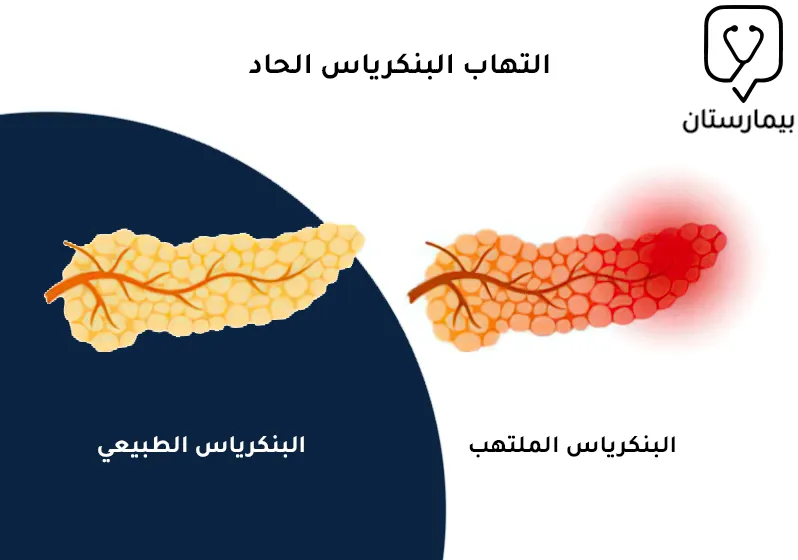
كثيراً ما يتعرض البنكرياس لحدوث الالتهاب لأسباب عديدة، وقد يكون التهاب البنكرياس حاد أو مزمن، بمعنى أن أعراض التهاب البنكرياس قد تظهر بشكل مفاجئ في غضون أيام قليلة ويشفى المرض بسرعة عند علاجه (الالتهاب الحاد)، وقد يتظاهر التهاب البنكرياس على شكل أعراض وعلامات لفترة زمنية طويلة تدوم لعدة سنوات (الإلتهاب المزمن).
يعرف البنكرياس بأنه عبارة عن غدة طويلة تقع في منقطة البطن خلف المعدة، تقوم هذه الغدة بإفراز إنزيمات وعصارات هاضمة تساعدك على هضم الطعام، إضافةً لدوره بإنتاج هرمون الأنسولين والغلوكاغون اللذان يعملان على ضبط مستوى سكر الدم لديك وإبقائه ضمن الحدود الطبيعية، لنتعرف أكثر على حالة التهاب البنكرياس وأعراضه الحادة والمزمنة مع أسبابه.
ما هي أعراض التهاب البنكرياس الحاد؟
بالنسبة لأعراض التهاب البنكرياس الحاد فهي قد تكون خفيفة أو شديدة بحسب شدة الإصابة الالتهابية، إذ يعاني بعض المرضى من أعراض بسيطة لا تشكل خطورة كبيرة وتتحسن بسرعة مع تلقي العلاج وعادةً ما تكون هذه الحالة هي الأكثر شيوعاً، بينما قد يكون الالتهاب أكثر شدة في بعض الحالات الأخرى ويؤدي لوقوع مضاعفات خطيرة مثل تنخر البنكرياس أو تحول الالتهاب للنوع المزمن.
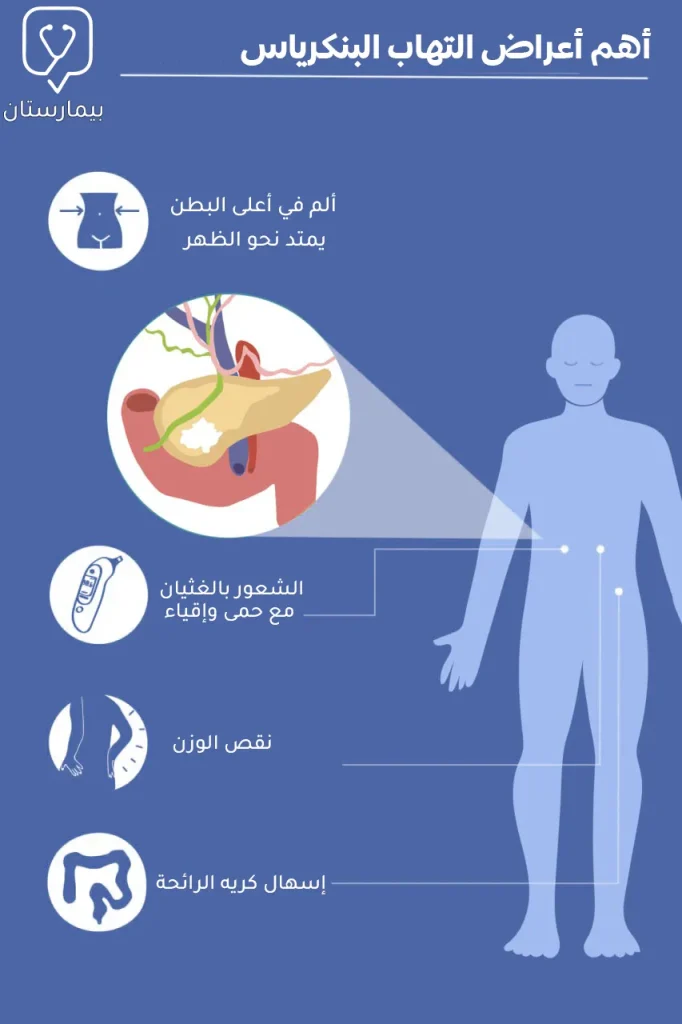
تشمل علامات التهاب البنكرياس الحاد ما يلي:
ألم البطن العلوي الذي يمتد باتجاه الظهر
غالباً ما يشكل ألم البطن أول الأعراض التي يشعر بها مرضى التهاب البنكرياس، يظهر الألم فجأة في النوع الحاد من التهاب البنكرياس ويتوضع في أعلى البطن وقد يمتد حتى يصل إلى منطقة الظهر، عادة ما يكون شديد للغاية وتزداد شدته عند لمس بطن المصاب أو بعد تناول الطعام.
الغثيان والإقياء
الشعور بالغثيان والقيء هي من الأعراض الشائعة لالتهاب البنكرياس الحاد، وقد تترافق مع أعراض أخرى كتسارع نبضات القلب وكذلك زيادة عدد مرات التنفس وعمقه.
ارتفاع الحرارة (الحمى)
كما هو الحال في معظم التهابات الجسم فإن الترفع الحروري هو من أعراض التهاب البنكرياس الحاد الشائعة، فقد تصل درجة حرارة المريض إلى 39° وقد تترافق مع اليرقان (اصفرار في الجلد والعينين).
فقدان الشهية للطعام
نتيجة ألم البطن الذي تزداد شدة مع تناول الطعام يفقد مريض التهاب البنكرياس الرغبة في الأكل والشرب مما قد يؤدي إلى انخفاض سريع في الوزن، يشاهد هذا العرض بِشكل أوضح في التهاب البنكرياس المزمن.
أعراض التهاب البنكرياس المزمن
يعرف التهاب البنكرياس المزمن بأنه حدوث إصابة دائمة تسبب ضعف في أداء غدة البنكرياس لوظائفها المختلفة في الجسم مما يتظاهر على شكل أعراض عدة تدوم لفترات زمنية طويلة وقد تستمر مدى الحياة، إلا أنه يمكن السيطرة على هذه الأعراض باتباع العلاج المناسب.
الإصابة المزمنة للبنكرياس قد تحصل نتيجة اسباب عديدة من بينها التهابات البنكرياس الحادة المتكررة والتي قد تخلف أذية لا عكوسة بالبنكرياس أو نتيجة شرب كميات كبيرة من الكحول على مدى فترات طويلة والذي يقود مع الزمن إلى تخريش وإصابة البنكرياس.
فيما يخص علامات وأعراض التهاب البنكرياس ذو الطبيعة المزمنة فتكون على الشكل الآتي:
- نوبات متكررة من ألم في البطن تظهر بين حينٍ وآخر
- مع تقدم الالتهاب تصبح النوبات أكثر تواتراً وتستغرق وقتاً أطول لتشفى
- نقص غير مفسر في الوزن
- الإسهال الدهني ذو الرائحة الكريهة (لعدم إفراز البنكرياس للأنزيمات الهاضمة)
- مغص في البطن قد يترافق مع غثيان وإقياء
أسباب التهاب البنكرياس الحاد
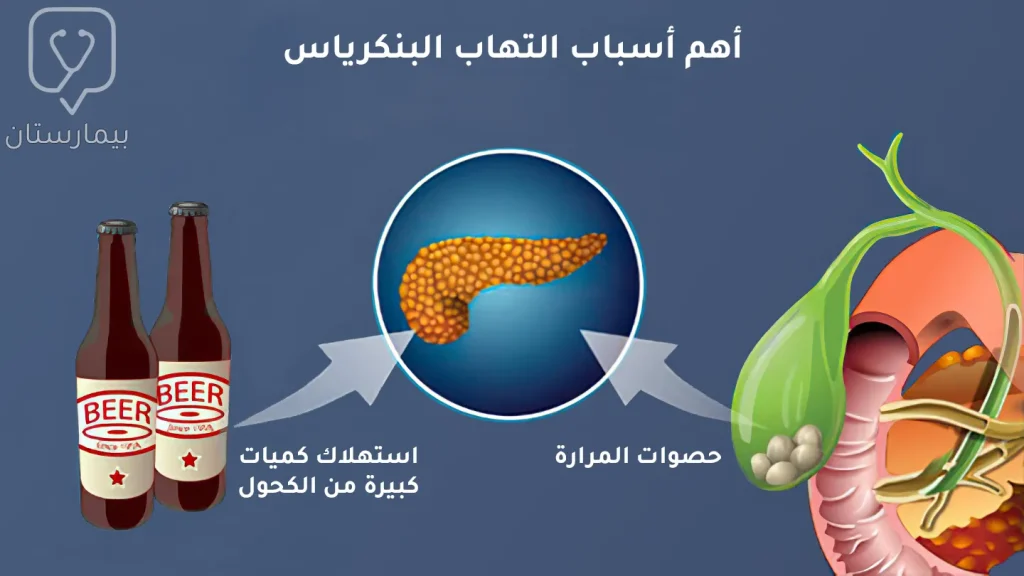
غالبًا ما يحدث التهاب البنكرياس نتيجة تنشيط الأنزيمات الهاضمة وهي ما تزال ضمن نسيج البنكرياس مما يسبب تخريش الخلايا البنكرياسية وحدوث الالتهاب الحاد.
يوجد عوامل خطورة تزيد من احتمال الإصابة وظهور أعراض التهاب البنكرياس الحاد ومن بينها ما يلي:
حصوات المرارة
تعتبر الحصوات المرارية من أكثر المسببات شيوعًا للإصابة بالتهابات البنكرياس، فقد تنزلق الحصيات الموجودة في المرارة وتقوم بسد القناة الصفراوية مما يتسبب باحتباس الإنزيمات ضمن البنكرياس.
إدمان الكحول
أثبتت الدراسات وجود علاقة وثيقة بين استهلاك كميات كبيرة من المشروبات الكحولية وزيادة خطر الإصابة بالتهاب البنكرياس، يعود السبب في ذلك لتأثير الكحول السام على الأقنية الصغيرة بالبنكرياس وخلايا Acinar البنكرياسية وزيادة لزوجة المفرزات مما يسبب انسداد بالأقنية واحتباس للأنزيمات.
الكحول قادر على إحداث التهاب حاد ومزمن بالبنكرياس ولكنه يعد مسؤول أكبر عن التهاب البنكرياس المزمن.
الاضطرابات الاستقلابية
ارتفاع الشحوم الثلاثية والكولسترول هما من عوامل الخطورة لالتهاب البنكرياس وذلك بسبب آلية التأثير على الدوران الدموي بالأوعية الشعرية الدقيقة مما يسبب إقفار في تروية خلايا البنكرياس، وكذلك الأمر في حالة فرط الكالسيوم.
استخدام بعض الأدوية
قد تسبب العقاقير الطبية عند البعض حدوث التهاب في غدة البنكرياس كأحد الآثار الجانبية المحتملة لهذه الأدوية وخاصة عندما تأخذ بجرعات مفرطة دون استشارة الطبيب ومن بين هذه الادوية ما يلي:
- المضادات الحيوية
- الستيروئيدات القشرية
- الأدوية الخافضة للضغط
- المدرات البولية
يوجد الكثير من المجموعات الدوائية القادرة على احداث التهاب بالبنكرياس، فعندما يتم تشخيص إصابتك بالتهاب البنكرياس سيسألك الأخصائي عن قيامك بأخذ أدوية جديدة مؤخراً.
الرضوض والجراحات السابقة
التعرض لحادث اصطدام مروري أو السقوط من ارتفاع شاهق على البطن قد يسبب أذية بالبنكرياس وكذلك الأمر في جراحات البطن التي تحمل خطر إصابة خاطئة للبنكرياس.
أسباب التهاب البنكرياس المزمن
يحدث التهاب البنكرياس المزمن عند تعرض البنكرياس لإصابة دائمة تؤدي إلى فشله بالقيام بوظائفه الطبيعية في الجسم وبالتالي تظهر الأعراض المزمنة للالتهاب والتي عادةً ما تستمر لسنوات عدة.
إن أهم وأشيع سبب لالتهاب البنكرياس المزمن عند البالغين هو الإفراط في استهلاك الكحول على مدى سنوات طويلة وذلك من خلال إحداث التهابات حادة متكررة تؤدي مع مرور الوقت لأذية البنكرياس وإصابته الدائمة.
أما بالنسبة للالتهاب المزمن الذي يصيب الأطفال فإن السبب الأشيع والأهم لحدوثه هو مرض التليف الكيسي Cystic fibrosis وهو من الأمراض الوراثية التي يولد الطفل بها وتسبب تضرر أعضاء عديدة بالجسم من بينها البنكرياس.
التهاب البنكرياس المناعي يعتبر أيضًا من الأسباب المهمة للإصابة الالتهابية المزمنة، فقد تهاجم مناعة جسمك المضطربة خلايا البنكرياس الطبيعية وتؤدي إلى التهاب في بنكرياسك.
ما تزال 20 إلى 30% من التهابات البنكرياس المزمنة مجهولة السبب، ولكن قام الأطباء بوضع عوامل خطورة قد ترفع من خطر إصابتك بالالتهاب ومنها:
- التدخين
- إصابة فرد من أفراد عائلتك بالتهاب البنكرياس
- زيادة الوزن والسمنة
- الداء السكري
- المعالجة الإشعاعية لمنطقة البطن
كيف يتم تشخيص التهاب البنكرياس
للتحري عن التهاب البنكرياس يقوم الأخصائي بالاستفسار عن أعراضك وطبيعة الألم الذي تعاني منه، ومن ثم يقوم بإجراء فحص جسدي عبر الضغط على البطن لمراقبة ردود فعلك وفي حال ازداد ألم بطنك أم لا.
يتم طلب أحد الاختبارات التالية لتأكيد التشخيص:
الاختبارات الدموية
عندما يصاب البنكرياس بالالتهاب تزداد نسبة أنزيماته بالدم خاصةً أنزيما الأميلاز والليباز، لذا يتم قياس نسبة كلا الأنزيمين بالدم فارتفاعهم يزيد الشك باحتمال إصابة البنكرياس إلا أنه ليس بالضرورة أن يشير الارتفاع دائماً لوجود الالتهاب.
يفيد أيضاً فحص تعداد الكريات البيض والفحوصات الدموية الأُخرى في التوجه نحو إلتهاب البنكرياس.
إيكو البطن
فحص البطن بالأمواج فوق الصوتية (الإيكو) هو من الوسائل المساعدة في التشخيص حيث يتمكن الفاحص عبره من التحري عن تغيرات التهابية بالبنكرياس أو تجمع الحصوات في المرارة.
التصوير الطبقي المحوري
يعطي الطبقي المحوري CT scan صورة واضحة لأعضاء البطن كالبنكرياس والمرارة للبحث والتحري عن التهابات أو حصيات مرارية.
خزعة البنكرياس
من النادر أن يتم طلب الخزعة وذلك لأن الاختبارات السابقة تكون كافية عادةً لتشخيص التهاب البنكرياس، غالباً ما تطلب الخزعة عند الشك بوجود سرطان البنكرياس حتى يتم نفيه.
تحليل البراز
يطلب هذا الفحص في حالة التهاب البنكرياس المزمن من أجل قياس مستويات الدهون في براز المريض والتي قد تشير إلى عدم امتصاص الطعام جيداً نتيجة خلل في عصارات البنكرياس الهاضمة.
ختاماً فإن أعراض التهاب البنكرياس الحاد والمزمن تتشابه نوعاً ما من حيث الطبيعة ولكنها تختلف عن بعضها بالشدة والفترة اللازمة لزوال الأعراض، فنجد أن اعراض التهاب البنكرياس المزمن تدوم لفترة أطول لكنها تكون أخف شدة بالمقارنة مع أعراض التهاب البنكرياس الحاد، وفي كلا النوعين يكون ألم البطن الممتد نحو الظهر هو العرض الأشيع، أما بالنسبة للأسباب فهي أيضاً متشابهة إذ تعتبر حصى المرارة والكحول هما أشيع المسببات لالتهاب البنكرياس.
المصادر:

